 Nov, 12 2025
Nov, 12 2025
Epinephrine Dosing Calculator
Determine Your Epinephrine Dose
This tool calculates the correct epinephrine dose based on weight. Always consult your doctor for personalized medical advice.
Critical Reminder
Never wait for multiple symptoms. If you have a known allergy and experience any sign of a serious reaction, give epinephrine immediately. Even if symptoms seem mild, epinephrine should be administered right away if you've been exposed to your allergen.
Carrying the right medications for an allergic reaction isn’t just smart-it can save your life or someone else’s. An allergy action plan isn’t a suggestion. It’s a clear, written guide that tells you exactly what to do when symptoms start. Too many people wait too long. They think hives or a runny nose aren’t serious. They reach for antihistamines first. But if it’s anaphylaxis, every second counts. Epinephrine is the only medication that can stop a life-threatening reaction. And it has to be given fast.
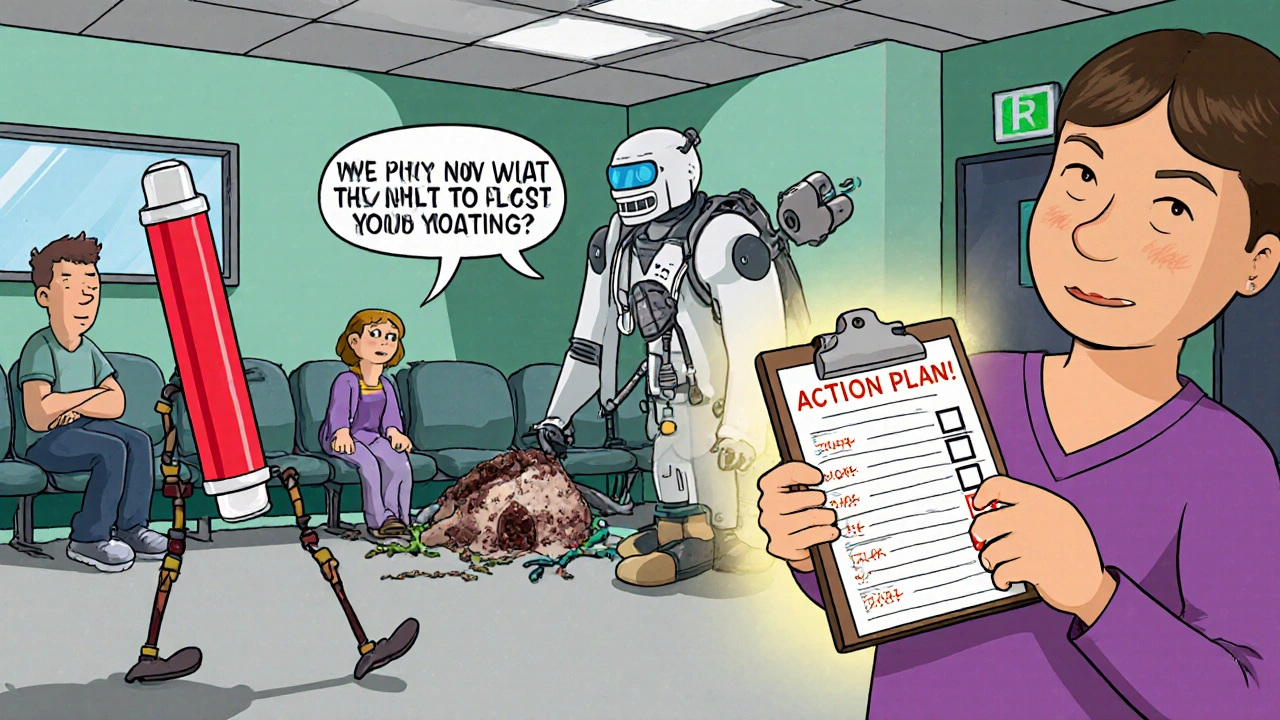
What’s in a Real Allergy Action Plan?
A true allergy action plan comes from your doctor. It’s not something you download off the internet and fill in yourself. It includes your name, your specific allergens, and a step-by-step guide based on your history. The most important part? It clearly states when to use epinephrine and when to call 911.
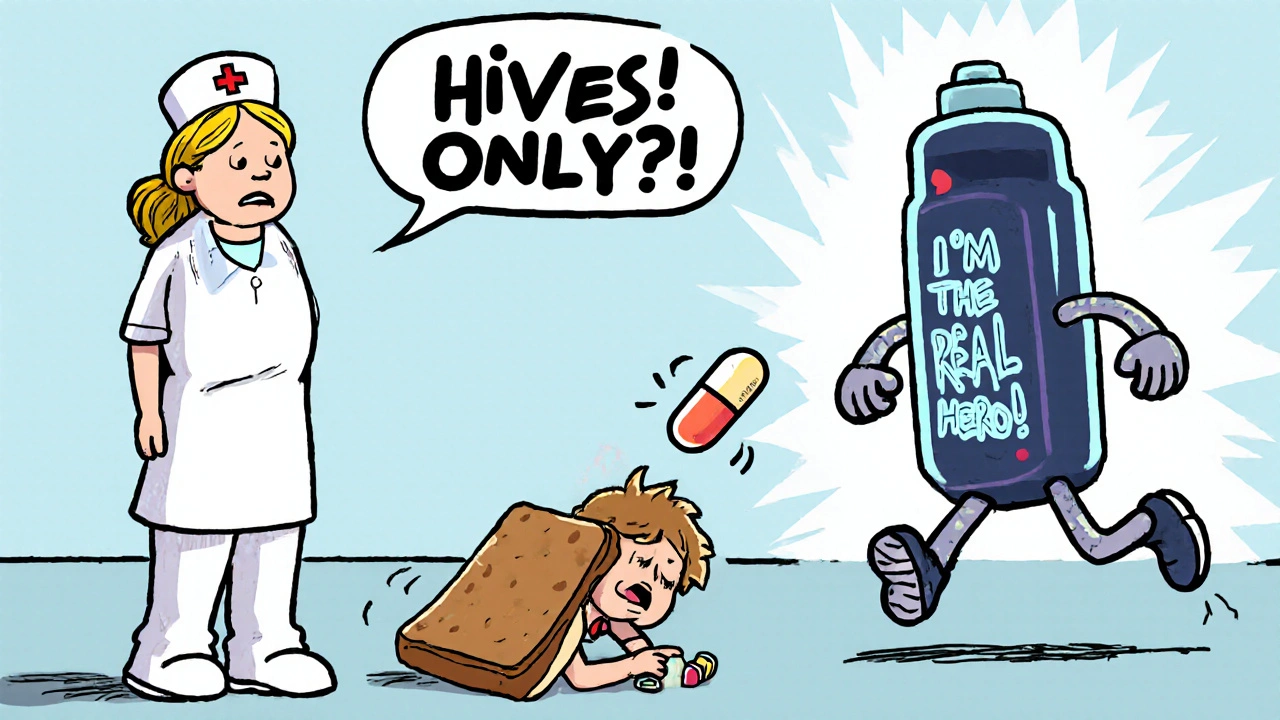
Every plan, whether from the American Academy of Pediatrics, FARE, or ASCIA, agrees on one thing: epinephrine is the first and only medication that stops anaphylaxis. It works by tightening blood vessels, opening airways, and supporting heart function. Antihistamines? They help with itching or hives. But they do nothing for swelling in the throat, low blood pressure, or trouble breathing. Relying on them alone is dangerous.
Doctors use weight to determine the right epinephrine dose:
- 7.5-13 kg (16.5-28.7 lbs): 0.10 mg
- 13-25 kg (28.7-55.1 lbs): 0.15 mg
- 25 kg+ (55.1 lbs+): 0.30 mg
Most people carry an auto-injector like EpiPen, Adrenaclick, or Auvi-Q. These are pre-measured and easy to use. But they expire. Check the date every time you refill. A 2023 FARE survey found 32% of households had expired epinephrine. That’s not a risk you can afford.
When to Use Epinephrine-No Exceptions
You don’t need to wait for multiple symptoms. If you’ve been exposed to your known allergen-like peanuts, shellfish, or bee venom-and you have any sign of a serious reaction, give epinephrine right away.
The medical definition of anaphylaxis? Two or more body systems reacting at once. For example:
- Skin: hives, swelling, flushing
- Respiratory: wheezing, throat tightness, coughing
- Cardiovascular: dizziness, fainting, rapid pulse
- Gastrointestinal: vomiting, diarrhea, cramps
But here’s the catch: if you’ve had anaphylaxis before, or if you have asthma, you’re at higher risk. In those cases, even one symptom after exposure means epinephrine. No waiting. No second-guessing.
For young children under 3, symptoms can be subtle. Sudden hives, persistent cough, or unusual lethargy aren’t normal. If they’ve eaten something they’re allergic to and act off, give epinephrine. Infants can’t tell you they’re struggling to breathe. You have to act.
There’s one exception: if someone has only hives or mild itching with no other symptoms, you might wait. But only if you’re watching closely. Give an antihistamine if your doctor approved it. But if even one more symptom shows up-swelling, vomiting, wheezing-give epinephrine immediately. Don’t delay.
What About Antihistamines?
Antihistamines like diphenhydramine (Benadryl) have a role-but only as a helper, not a hero. They’re fine for mild reactions: a few hives, itchy mouth, sneezing. But they do not stop anaphylaxis. They don’t open airways. They don’t raise blood pressure. And if you give them first, you might delay epinephrine.
A 2021 study found that in school settings, people who reached for antihistamines first waited an average of 22 minutes longer to give epinephrine. That’s 22 minutes where the reaction can get worse. In one case, a child with peanut allergy had hives. The teacher gave Benadryl. Ten minutes later, the child started vomiting. By then, it was too late. Epinephrine was given, but the delay made recovery harder.
Use antihistamines only after epinephrine, or for mild symptoms with no risk of progression. Never use them instead of epinephrine.
What Else Should You Carry?
Alongside epinephrine, most plans recommend:
- Antihistamines: Oral diphenhydramine or cetirizine. Dose is 1 mg per kg of body weight, up to 50 mg max. Keep them in a separate, labeled container.
- Albuterol inhaler: If you have asthma or get wheezing during reactions. Use it after epinephrine if breathing is still tight.
- Medical ID bracelet: It tells strangers what’s wrong if you can’t speak. Include your allergens and that you carry epinephrine.
- Written copy of your plan: Keep one in your wallet, one in your child’s backpack, and give one to school, daycare, or work. Make sure it’s signed by your doctor.
Some newer options are emerging. In 2023, the FDA approved Neffy, an intranasal epinephrine spray. It’s not for everyone-it’s not yet recommended for children under 12 or people with severe nasal congestion. But for adults who fear needles, it’s an option. Ask your allergist if it’s right for you.
What Happens After You Give Epinephrine?
Calling 911 isn’t optional. Even if you feel better after the shot, you still need to go to the hospital. About 20% of people have a second wave of symptoms-called a biphasic reaction-up to 12 hours later. That’s why you need to be monitored for 4 to 6 hours.
Don’t assume one dose is enough. If symptoms return or don’t improve after 5-10 minutes, give a second dose of epinephrine. Yes, you can give more than one. Auto-injectors are designed for this. Many people hesitate because they think it’s dangerous. It’s not. The risk of not giving it is far greater.
Keep your epinephrine with you at all times. Not in the glovebox. Not at home. Not in the office. Carry it on your person. Pockets, waistbands, or a dedicated bag you never leave behind. If you’re going to a restaurant, a park, or a friend’s house-bring it. Reactions don’t wait for convenience.
Common Mistakes and How to Avoid Them
People mess up in predictable ways:
- Waiting for “worse” symptoms: If you have a known allergy and you’re reacting, don’t wait for the throat to close. Give epinephrine at the first sign.
- Not checking expiration dates: Replace auto-injectors before they expire. Even if they look fine, the medicine degrades.
- Not training others: Teachers, babysitters, coworkers-show them how to use the injector. Practice on a trainer device. Most schools now require training, but 38% of teachers still can’t recognize anaphylaxis without a visual guide.
- Leaving plans at home: If your child has a plan, make sure the school has a copy. Keep one in your phone as a photo backup.
- Thinking antihistamines prevent reactions: They don’t. They only treat symptoms after they start.
Parents often say they feel more confident with a written plan. One survey found 87% of families felt safer after getting a doctor-approved action plan. But 63% still struggle with school staff not taking it seriously. Bring the plan to every meeting. Ask for a copy of the school’s allergy policy. If they won’t follow it, escalate it.
Digital Plans Are Changing the Game
More people are using apps now. FARE launched a mobile app in March 2024 that lets you store your action plan, set expiration alerts for epinephrine, and share emergency contacts with one tap. Over 142,000 people use it. It’s not a replacement for a printed copy-but it’s a powerful backup.
Some hospitals are testing AI tools that can spot anaphylaxis from video. Stanford’s 2023 pilot showed 92% accuracy identifying symptoms from phone footage. In the future, these tools might link to digital plans and automatically alert emergency services. But for now, the best tool is still a clear, printed plan-and the courage to use it.
Your Action Plan Checklist
Before you leave the house, ask yourself:
- Do I have my epinephrine auto-injector? (Check expiration date)
- Do I have a backup dose?
- Do I have antihistamines? (Only if approved by doctor)
- Do I have my written plan? (Printed copy or photo on phone)
- Have I shown someone how to use the injector? (Partner, teacher, coworker)
- Do I know the signs of a severe reaction?
If you answer yes to all, you’re ready. If not, fix it now. Don’t wait for an emergency to realize you’re unprepared.
Can I use an antihistamine instead of epinephrine for a severe reaction?
No. Antihistamines like Benadryl only help with mild symptoms like itching or hives. They do not stop airway swelling, low blood pressure, or shock-the life-threatening parts of anaphylaxis. Epinephrine is the only medication that can reverse these effects. Delaying epinephrine to give antihistamines first increases the risk of death.
What if I’m not sure if it’s an allergic reaction?
If you’ve been exposed to a known allergen and you’re experiencing any unusual symptoms-especially breathing trouble, dizziness, swelling, or vomiting-give epinephrine. It’s safer to use it when you’re unsure than to wait and risk a fatal reaction. Epinephrine is very safe for most people. Side effects like a racing heart or shaking are temporary and far less dangerous than untreated anaphylaxis.
How often should I replace my epinephrine auto-injector?
Replace your epinephrine auto-injector before the expiration date printed on the device. Most last 12 to 18 months. Even if the liquid looks clear and the device hasn’t been used, the medicine loses potency over time. Set a reminder on your phone 30 days before expiration. Many pharmacies will help you track this when you refill.
Do I need to carry epinephrine if I’ve never had a severe reaction before?
Yes-if you have a known allergy that could cause anaphylaxis, like peanut, tree nut, shellfish, or insect venom allergies. First reactions can be severe. Studies show half of all fatal food allergy reactions happen on the first known exposure. Having epinephrine doesn’t mean you expect a reaction. It means you’re prepared in case one happens.
Can I use someone else’s epinephrine auto-injector?
Yes, if it’s the right dose for the person having the reaction. Epinephrine auto-injectors are not personalized by name-they’re dosed by weight. A 0.3 mg injector is safe for most adults and teens. If you’re helping someone with a known allergy and they don’t have their own, use yours. It’s better than nothing. Many states have Good Samaritan laws that protect people who help in emergencies.
Is there a difference between epinephrine brands like EpiPen and Auvi-Q?
The medicine inside is the same. The main differences are how they work. EpiPen has a spring-loaded needle you press into the thigh. Auvi-Q gives voice instructions during use. Neffy is a nasal spray. Choose the one you’re most comfortable with and practice with a trainer device. The most important thing is knowing how to use yours quickly under stress.
Should I carry epinephrine if my child has a mild allergy?
Yes-if your child has been diagnosed with a food or insect allergy that could lead to anaphylaxis, even if past reactions were mild. Allergies can get worse with each exposure. A mild reaction today doesn’t guarantee a mild one tomorrow. The American Academy of Pediatrics recommends epinephrine for anyone with a history of anaphylaxis or a known allergen with potential for severe reaction, regardless of past severity.

Chrisna Bronkhorst
November 13, 2025 AT 00:05Eve Miller
November 13, 2025 AT 12:25Amie Wilde
November 14, 2025 AT 19:25Rashmi Mohapatra
November 16, 2025 AT 09:27Renee Ruth
November 17, 2025 AT 12:46Esperanza Decor
November 19, 2025 AT 02:45Alex Ramos
November 19, 2025 AT 12:48Samantha Wade
November 19, 2025 AT 22:28Alyssa Lopez
November 20, 2025 AT 08:56edgar popa
November 20, 2025 AT 12:48Gary Hattis
November 20, 2025 AT 23:18Andy Slack
November 21, 2025 AT 17:58