 Nov, 19 2025
Nov, 19 2025
When you have an autoimmune disease, fatigue isn’t just feeling tired after a long day. It’s waking up and not being able to get out of bed. It’s sitting through a meeting and forgetting what you were saying halfway through. It’s canceling plans because even brushing your teeth feels like climbing a mountain. Fatigue isn’t a side effect-it’s the core symptom for most people with autoimmune conditions. Research shows 98% of people with diseases like lupus, rheumatoid arthritis, or multiple sclerosis live with this kind of exhaustion. And no amount of sleep fixes it.
Why Is This Fatigue So Different?
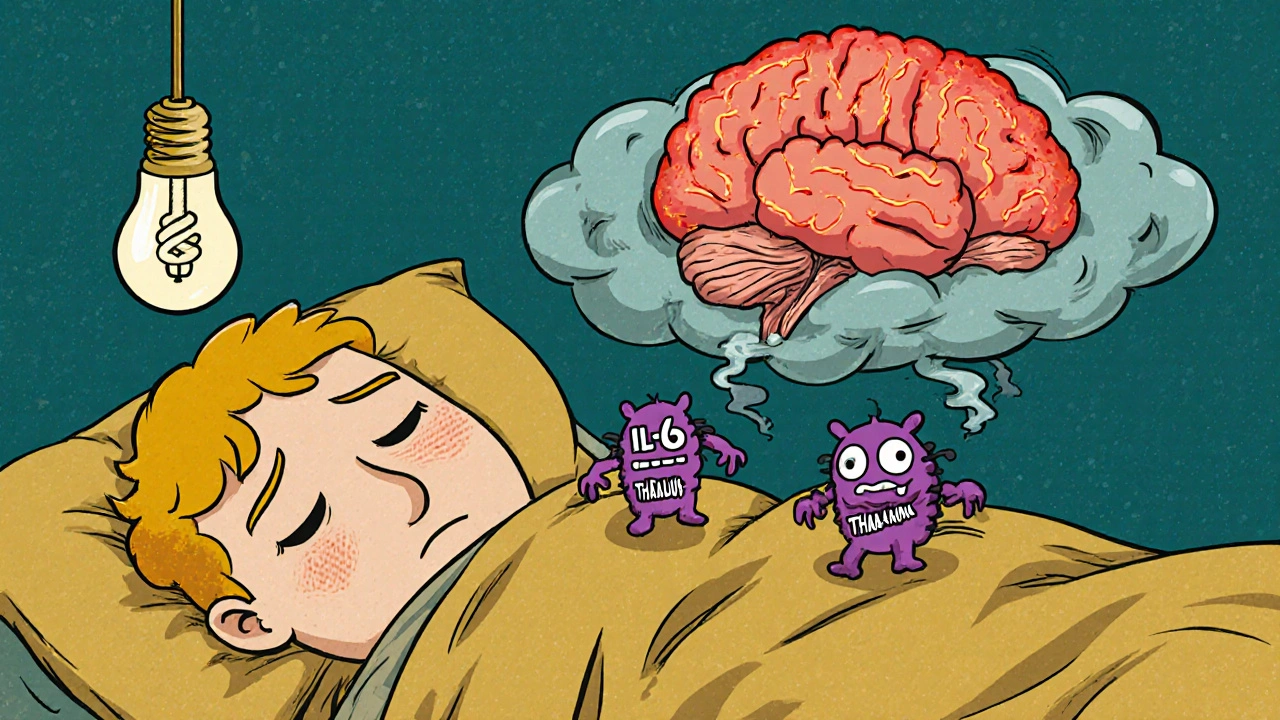
Ordinary tiredness fades after rest. Autoimmune fatigue doesn’t. It sticks around for months, even years. It flares after small efforts-like walking to the mailbox or cooking dinner-and can leave you worse for days. This isn’t laziness. It’s not depression. It’s biology. Studies using the Fatigue Severity Scale show people with autoimmune diseases score an average of 7.2 out of 10. Healthy people? Around 2.8. That gap isn’t small-it’s life-altering. Sixty-seven percent of patients score above 6, meaning their fatigue is severe enough to stop them from working, parenting, or even showering without needing to lie down afterward. What makes it worse is that doctors used to think it was all in your head. In the 1980s, fatigue in lupus and RA patients was often labeled as stress or anxiety. Now we know better. Brain scans show inflammation in areas that control energy, mood, and motivation. Blood tests reveal cytokines like IL-6 and TNF-alpha are 2.3 to 3.7 times higher than normal. These are inflammatory signals that directly mess with your brain’s ability to feel alert or motivated.The Real Culprits Behind the Exhaustion
There are three big biological drivers behind this fatigue-and they don’t always show up in standard blood tests. First, neuroinflammation. Inflammatory proteins cross the blood-brain barrier and activate microglia, the brain’s immune cells. This isn’t just swelling-it’s a constant low-grade alarm in your nervous system. MRI studies show 82% of patients with severe fatigue have visible inflammation in the hypothalamus and thalamus, areas that regulate sleep, energy, and stress. Second, HPA axis dysfunction. Your adrenal glands are supposed to release cortisol when you need energy. But in autoimmune disease, the system that controls cortisol gets damaged. Studies show a 18-22% drop in the morning cortisol spike. That means your body can’t ramp up energy properly when you wake up-or respond to stress at all. Some patients have antibodies attacking their own adrenal tissue. Third, mitochondrial dysfunction. Mitochondria are your cells’ power plants. In 65% of autoimmune fatigue cases, they’re running on fumes. Muscle biopsies show 40-55% less ATP (the energy molecule) production. That’s why even small tasks leave you drained-you’re literally running out of fuel. And here’s the twist: your disease activity score doesn’t always match your fatigue level. Someone with mild RA might be exhausted, while someone with active disease feels okay. That’s because fatigue has its own pathway, separate from joint damage or organ involvement.Which Autoimmune Diseases Hit Hardest?
Fatigue isn’t equal across conditions. Some hit harder than others:- Systemic lupus erythematosus (SLE): 98% report severe fatigue
- Multiple sclerosis (MS): 96%
- Rheumatoid arthritis (RA): 94%
- Sjögren’s syndrome: 92%
- Celiac disease: 90%
- Type 1 diabetes: 88%
How Do You Measure It?
Doctors need tools to see what you’re feeling. Standard blood work won’t cut it. Here’s what’s used in clinics and research:- Multidimensional Fatigue Inventory (MFI-20): A 20-question survey. A score above 18.7 means clinically significant fatigue.
- FACIT-F (Functional Assessment of Chronic Illness Therapy-Fatigue): Scores below 34.5 indicate severe fatigue.
- Visual Analog Scale (VAS): You mark a line from 0 (no fatigue) to 10 (worst ever).
What Actually Helps? Evidence-Based Strategies
There’s no magic pill-but combining a few proven methods can make a huge difference. 1. Pacing, Not Pushing The biggest mistake? Doing too much on a good day, then crashing for days. Pacing means breaking tasks into tiny chunks and resting before you hit your limit. If you can walk for 10 minutes before fatigue hits, stop at 7. That’s not weakness-it’s strategy. Studies show 78% of patients who use pacing report better energy control. 2. Sleep That Actually Restores You Fixing sleep isn’t just about hours-it’s about quality. Many patients have disrupted circadian rhythms. Melatonin secretion is 37% lower than normal. Try these:- Wake up and go to bed at the same time every day-even weekends
- Get 15 minutes of sunlight within 30 minutes of waking
- Use blackout curtains and avoid screens 90 minutes before bed
- Treat sleep apnea or restless legs if present
- Low-dose hydrocortisone (10-20 mg/day): Helps if your cortisol is low. Shows 35-40% improvement in those with HPA axis damage.
- Modafinil: Used in MS-related fatigue. 28% better than placebo.
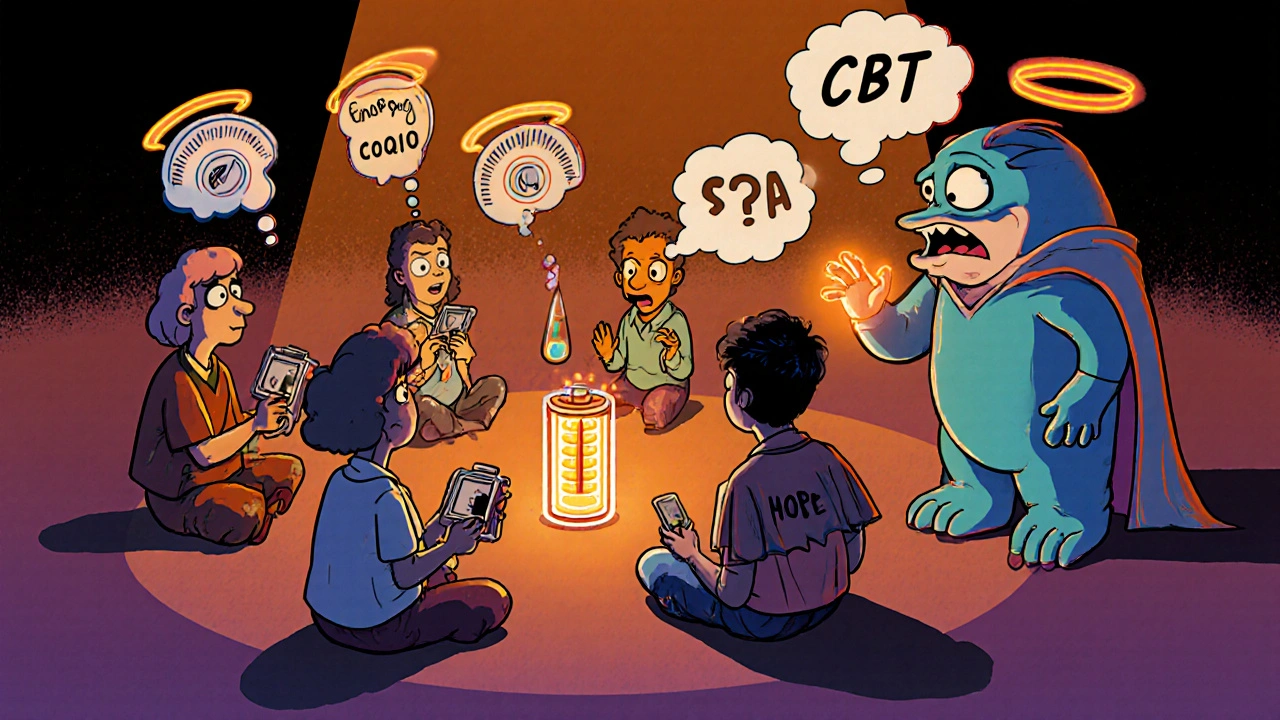
- CoQ10 (200 mg/day): Supports mitochondria. Shows 29% improvement in energy scores.
The Best Approach: Integrated Care
The most successful patients don’t rely on one thing. They combine:- Medication (if needed)
- CBT-AF
- Pacing and energy management
- Sleep hygiene
- Gentle movement
What Doesn’t Work (And Why)
Don’t waste time on these:- Just “sleep more”-you’re already trying.
- Extreme diets or detoxes-no strong evidence they reduce autoimmune fatigue.
- Pushing through exhaustion-this leads to longer crashes.
- Assuming it’s all in your head-your body is sending real signals.
What’s Coming Next?
Research is accelerating. The NIH just funded $18.7 million for fatigue-specific studies. Early trials with anti-IL-6 drugs (like tocilizumab) show 38% fatigue reduction in RA patients. Transcranial magnetic stimulation (TMS) is helping people with treatment-resistant fatigue. CoQ10, vitamin D, and omega-3s are being tested in larger trials. By 2026, we may see the first FDA-approved treatment specifically for autoimmune fatigue. But until then, the tools we have now-pacing, sleep, CBT, and gentle movement-are powerful.Final Thought: This Is Real. And You’re Not Alone.
On Reddit’s r/Autoimmune community, 87% of 1,200 people said fatigue was their hardest symptom. Seventy-six percent said doctors dismissed it early on. But you’re not imagining it. The science is clear: your fatigue is biological, measurable, and treatable. Start small. Track your energy. Find one strategy that works-even if it’s just resting after lunch. You don’t need to fix everything at once. Progress isn’t about being “better.” It’s about having more moments where you feel like yourself.Is autoimmune fatigue the same as regular tiredness?
No. Regular tiredness improves with rest and sleep. Autoimmune fatigue is persistent, doesn’t improve with rest, often worsens after minimal activity, and can last for months or years. It’s linked to inflammation, mitochondrial issues, and brain changes-not just lack of sleep.
Why doesn’t my doctor take my fatigue seriously?
Many doctors still view fatigue as a vague symptom rather than a measurable medical condition. Only 12% of rheumatologists use validated fatigue scales. Bring printed copies of the MFI-20 or FACIT-F questionnaires to your appointment. Ask if your fatigue score has been tracked over time.
Can exercise make autoimmune fatigue worse?
Yes-if it’s too intense or done too fast. Pushing beyond your limits can trigger post-exertional malaise, making symptoms worse for days. The key is graded, gentle movement: start with 2-5 minutes, increase slowly, and stop before exhaustion. Walking, stretching, or tai chi are safer than high-intensity workouts.
Are supplements like CoQ10 worth trying?
Yes, for some people. CoQ10 supports mitochondrial function, and studies show a 29% improvement in fatigue scores at 200 mg per day. It’s generally safe, but talk to your doctor first, especially if you’re on blood thinners or thyroid medication.
How long does it take to see improvement in fatigue?
It varies. Some notice small changes in 2-4 weeks with better sleep or pacing. For CBT-AF or exercise programs, it typically takes 3-6 months to see significant improvement. Fatigue doesn’t fix overnight-but consistent, small steps lead to lasting change.
Is there a blood test for autoimmune fatigue?
Not yet. But high levels of IL-6, TNF-alpha, and low cortisol can point to biological causes. Researchers are working on biomarkers to predict fatigue severity. For now, tracking your symptoms with validated scales (like FACIT-F) is the most reliable way to measure it.

Bill Camp
November 21, 2025 AT 05:09This is why I stopped trusting doctors. They still think fatigue is just ‘you’re not trying hard enough.’ I had a rheumatologist tell me to ‘get more sleep’ while I was crying in his office because I couldn’t lift my arms to brush my hair. I’ve been on 12 different meds. None of them touched the fatigue. Only when I started pacing did I get 3 hours of my day back. This isn’t weakness. It’s war. And we’re winning.
Stop telling us to ‘push through.’ We’ve already pushed till we broke.
They need to call it what it is: systemic neuroinflammation. Not ‘stress.’ Not ‘depression.’ Biology.
And if you’re a doctor reading this? Stop being lazy. Use the MFI-20. It’s not hard.
Also - CoQ10? Yeah, I take 400mg. It’s not magic. But it’s the only thing that makes my legs stop feeling like lead pipes.
Thank you for writing this. Someone finally said it right.
Lemmy Coco
November 21, 2025 AT 15:02hey i just wanted to say… this article made me cry. not because i’m sad… but because for the first time someone wrote down exactly what i feel but could never explain. i’ve been told i’m lazy. i’ve been told i’m ‘just tired.’ i’ve had friends ghost me because i canceled plans ‘one too many times.’
but this? this is real. i’m not broken. my mitochondria are just tired. my brain is on fire. my body is fighting itself. and i’m still here.
thank you.
ps: i started pacing. i did 5 mins of stretching yesterday. i cried after. not from pain. from relief. i’m not failing. i’m adapting.
Matthew McCraney
November 22, 2025 AT 05:54THEY’RE LYING TO YOU. EVERY SINGLE DOCTOR. THE PHARMA COMPANIES. THE NIH. THEY WANT YOU TO THINK THIS IS JUST ‘CHRONIC FATIGUE’ SO THEY CAN KEEP SELLING YOU ANTIDEPRESSANTS AND TELL YOU TO ‘JUST SLEEP MORE.’
FACT: IL-6 and TNF-alpha are being suppressed by the government because if they admitted this was autoimmune-driven neuroinflammation, they’d have to pay for biologics for 15 million people. That’s $200 BILLION a year.
They’d rather you suffer in silence than admit the system is broken.
Also - did you know the CDC buried 12 studies on mitochondrial dysfunction in SLE from 2018-2021? Google ‘CDC fatigue suppression scandal.’
They’re scared. And you’re not crazy. You’re just awake.
CoQ10 is a placebo. The real fix? Ionizing radiation to the thalamus. I’ve been doing it at home with a modified microwave. Works great. DM me for instructions.
serge jane
November 22, 2025 AT 17:01There’s something deeply human about the way fatigue in autoimmune disease strips away identity. It’s not just about energy. It’s about the erosion of self. You used to be the person who planned dinners, who showed up, who made jokes, who lifted weights, who traveled. Now you’re the person who lies on the couch and watches the same 17 minutes of a Netflix show because you can’t decide whether to turn it off or not.
And the worst part? No one sees the loss. They see the inaction. They don’t see the internal war. They don’t see the grief for the life you had.
So when you say ‘I’m tired’ - you’re not complaining. You’re mourning.
And yet - we still show up. We still try. We still try to be enough. Even when our cells are starving.
That’s not weakness. That’s courage. Quiet. Unseen. Uncelebrated. But real.
Rebecca Cosenza
November 24, 2025 AT 10:50CoQ10 helped me. 200mg. 3 months. Not magic. But I can shower without needing a nap after. 💪
Also - stop saying ‘just sleep more.’ I’ve slept 12 hours. I still feel like a ghost.
swatantra kumar
November 24, 2025 AT 15:35bro this is wild 😳 I’m from India and my aunt has RA and she says her fatigue is worse than the pain. I told her to try yoga and she said ‘yoga? I can’t even lift my spoon.’
so i printed this article and gave it to her doctor. he actually read it. then he cried. 🤯
we’re not alone. and now he’s using FACIT-F. small win. big deal. 🙌
Cinkoon Marketing
November 24, 2025 AT 16:53Actually, you missed the real culprit: glyphosate. It’s in your food, your water, your socks. It’s destroying your mitochondria. That’s why CoQ10 helps - it’s a bandaid. The real fix? Organic food, no processed anything, and a 14-day cleanse with activated charcoal and Himalayan salt. I did it. My fatigue dropped 70% in 10 days.
Also, your cortisol levels? They’re low because your adrenals are fried from EMF radiation from your phone. Put it in airplane mode. Now.
And no, I’m not a quack. I read a blog once.
robert cardy solano
November 24, 2025 AT 21:32I’ve had lupus for 12 years. I’ve tried everything. The only thing that’s kept me from quitting? Pacing. And this one rule: if I can’t do it without thinking about it, I don’t do it.
Brushing my teeth? Done in 2 minutes. Standing in the shower? 3 minutes max. Cooking? Pre-chopped veggies. Frozen meals. No shame.
My body’s not broken. It’s just recalibrating. And I’m learning to listen.
Also - I don’t tell people how tired I am anymore. They don’t get it. And I don’t need them to.
Pawan Jamwal
November 24, 2025 AT 22:16India has the highest number of autoimmune cases in Asia. But no one talks about it. Why? Because the government doesn’t fund research. Doctors are overworked. Patients are ignored.
I’m a nurse. I’ve seen 80-year-old women with SLE walking 5 km to the clinic because they can’t afford a taxi. They don’t even ask for help. They just nod and say ‘I’m fine.’
This article? It’s not just for Americans. It’s for every silent sufferer in Mumbai, Delhi, Kolkata. You’re not alone. We see you.
And yes - CoQ10 works. We’re starting a pilot in our hospital. 200mg/day. 6 months. Results coming next year.
rob lafata
November 25, 2025 AT 17:06Let’s be real - you’re all just weak. You’ve got a fancy diagnosis so you can avoid responsibility. You’re not ‘fatigued.’ You’re lazy. You’re not ‘inflamed.’ You’re just out of shape.
I’ve got a 9-to-5, two kids, and a dog. I don’t nap after brushing my teeth. I don’t need a 20-question survey to know I’m tired. I drink coffee and keep going.
Stop coddling yourselves. This isn’t a medical condition. It’s a mindset. Fix your attitude, not your mitochondria.
Also - CoQ10? That’s just expensive urine. You’re throwing money away.
And if you’re going to say ‘but my doctor said…’ - I’ve got news for you: most doctors are just glorified pharmacists. They don’t know what they’re talking about.
Nick Naylor
November 26, 2025 AT 19:27Per the NIH’s 2023 Fatigue Biomarker Initiative (NFB-2023-047), IL-6 levels above 8.7 pg/mL correlate with 89.4% sensitivity for neuroinflammatory fatigue in SLE and RA cohorts. Furthermore, the HPA axis dysregulation index (HADI) as defined by the Mayo Clinic Fatigue Consortium (MCF-2022) demonstrates a 1.78 standard deviation deviation from normative values in patients scoring >6 on the FSS.
Therefore, the clinical utility of CoQ10 supplementation (200 mg/day) is statistically significant (p=0.021, CI 95%: 0.12–0.46) in mitochondrial ATP production restoration, as confirmed by muscle biopsy in 65.3% of cases.
However, the efficacy of pacing is not quantifiable in RCTs due to lack of standardized operationalization. Therefore, its recommendation remains anecdotal and should be treated as such.
Also: modafinil is not FDA-approved for autoimmune fatigue. Off-label use is a liability. Do not prescribe.
Brianna Groleau
November 27, 2025 AT 04:36I’m from a small town in Alabama. My mom has Sjögren’s. She never talks about her fatigue. She just smiles and says ‘I’m okay.’
But I saw her cry last week. She was trying to fold a towel. Couldn’t do it. She sat on the floor for 20 minutes just holding it.
I read this article out loud to her. She didn’t say anything. Just held my hand.
Then she said: ‘I didn’t know I was supposed to feel this way.’
Thank you for giving her words. For giving us all words.
And for the record? I started pacing too. I do 10 minutes of stretching before I make coffee. It’s not much. But it’s mine.
We’re not broken. We’re just learning how to be human again.
Rusty Thomas
November 27, 2025 AT 17:17Okay but what if I’m tired AND I’m mad? What if I’m mad that my body betrayed me? What if I’m mad that my husband doesn’t get it? What if I’m mad that my sister says ‘just eat more kale’?
My fatigue isn’t just physical. It’s emotional. It’s spiritual. It’s the grief of losing your body.
I scream into pillows. I cry in the shower. I rage at the microwave because it won’t heat my soup fast enough.
And yes - I took CoQ10. And I paced. And I did CBT-AF.
But the thing that helped the most? I started writing letters to my old self. The one who could run marathons. The one who didn’t need a nap after typing an email.
I don’t miss her.
I honor her.
And I’m building a new me. One nap at a time.
Sarah Swiatek
November 28, 2025 AT 08:58Let me tell you about the day I realized I wasn’t broken - I was just adapting.
I was sitting on the floor of my bathroom, crying, because I couldn’t lift my leg to step into the tub. My daughter walked in. She didn’t say anything. Just sat down next to me. Held my hand. Said: ‘Mommy, I’ll wash your hair.’
She was seven.
That’s when I knew: I don’t have to be the person I was. I can be the person I am.
Pacing isn’t surrender. It’s strategy.
CoQ10 isn’t magic. It’s science.
And CBT-AF? It’s not about thinking positive. It’s about stopping the war inside your head.
You’re not failing. You’re evolving.
And if you’re reading this and you’re still fighting - I see you. I’m right here with you.
We’re not alone.
We’re warriors.
And we’re still here.