 Nov, 20 2025
Nov, 20 2025
Every year, thousands of people in Australia get the wrong medicine-sometimes the wrong dose, sometimes the wrong drug entirely. It’s not because pharmacists are careless. It’s because mistakes happen in busy environments, even with the best systems. And while pharmacies have their own checklists to prevent errors, you can be the last line of defense. You don’t need to be a doctor or a pharmacist to catch a mistake. You just need a simple habit: a personal safety checklist for pharmacy visits.
Why You Need a Checklist
Pharmacies in Australia are required by law to follow strict safety rules. But rules don’t stop human error. A pharmacist might be distracted by a crying child, a system glitch, or a misread prescription. You might not notice the difference between amoxicillin and azithromycin-but if you’re taking one for a sinus infection and get the other, it won’t work. Or worse, it could cause side effects. The good news? You don’t need to memorize drug names or understand chemical formulas. You just need to ask the right questions and check a few basic things every time you pick up a prescription.Step 1: Know What You’re Supposed to Get
Before you even leave the house, open your phone or grab your prescription slip. Write down:- The full name of the medicine (e.g., Metformin 500mg, not just “diabetes pill”)
- The dose (e.g., once daily, two tablets)
- The reason you’re taking it (e.g., for high blood sugar)
- How long you’re supposed to take it (e.g., 30 days)
Step 2: Check the Label When You Get It
When the pharmacist hands you the medicine, pause. Don’t just take it and walk out. Look at the label. Does it match what you wrote down? Ask yourself:- Is the name spelled right? (Some names sound alike-Clonazepam vs. Clonidine)
- Is the dose correct? (Is it 5mg or 50mg?)
- Is the number of pills right? (Did they give you 30 when you need 60?)
- Is the instructions clear? (e.g., “Take with food” or “Take on an empty stomach”)
Step 3: Ask the “Three Questions” Every Time
These three questions take less than 30 seconds and can prevent a dangerous error:- “Is this the same medicine I’ve taken before?” If you’ve taken this drug before, does it look or taste the same? Pills change color, shape, or size when manufacturers switch. That’s normal-but you should know it.
- “What is this medicine for?” Even if you think you know, ask. Sometimes prescriptions get mixed up. A pill meant for high blood pressure might be labeled for cholesterol.
- “Are there any side effects I should watch for?” This isn’t just about safety-it’s about awareness. If you know to expect dizziness or nausea, you won’t panic if it happens.

Step 4: Compare With Your Old Bottle
If you’re refilling a prescription, bring the empty or half-used bottle with you. Lay it next to the new one. Do they match? - Same color? Same shape? Same imprint code? (That’s the number or letter stamped on the pill.) - Same expiration date? (If it’s way older than expected, that’s a red flag.) - Same pharmacy label format? (Different pharmacies use different templates.) If something looks different and you can’t explain why, ask. Sometimes a generic version is substituted-and that’s fine. But you should be told. If the pharmacist says, “It’s just a different brand,” ask them to confirm it’s the same active ingredient.Step 5: Use Your Phone to Document
Take a photo of the prescription label and the pill itself before you leave the pharmacy. Store it in a folder called “Medications.” Why? Because memory fades. A week later, you might forget if the blue pill was 10mg or 20mg. If you have a photo, you can show it to your doctor or another pharmacist if something feels wrong. It also helps if you need to report an error later. Don’t just take a picture of the bottle. Take one of the pill. The imprint code matters. You can even use apps like Drugs.com Pill Identifier to cross-check later.Step 6: Know When to Walk Away
If something feels off-your gut says no-don’t take the medicine. Say, “I’m not comfortable with this. Can I speak to the pharmacist again?” Pharmacies have a duty to resolve your concerns. If they brush you off, ask to speak to the manager. If you’re still not satisfied, call Healthdirect on 1800 022 222. They can help you figure out if there’s a real issue. You have the right to safe medication. No one should make you feel silly for asking.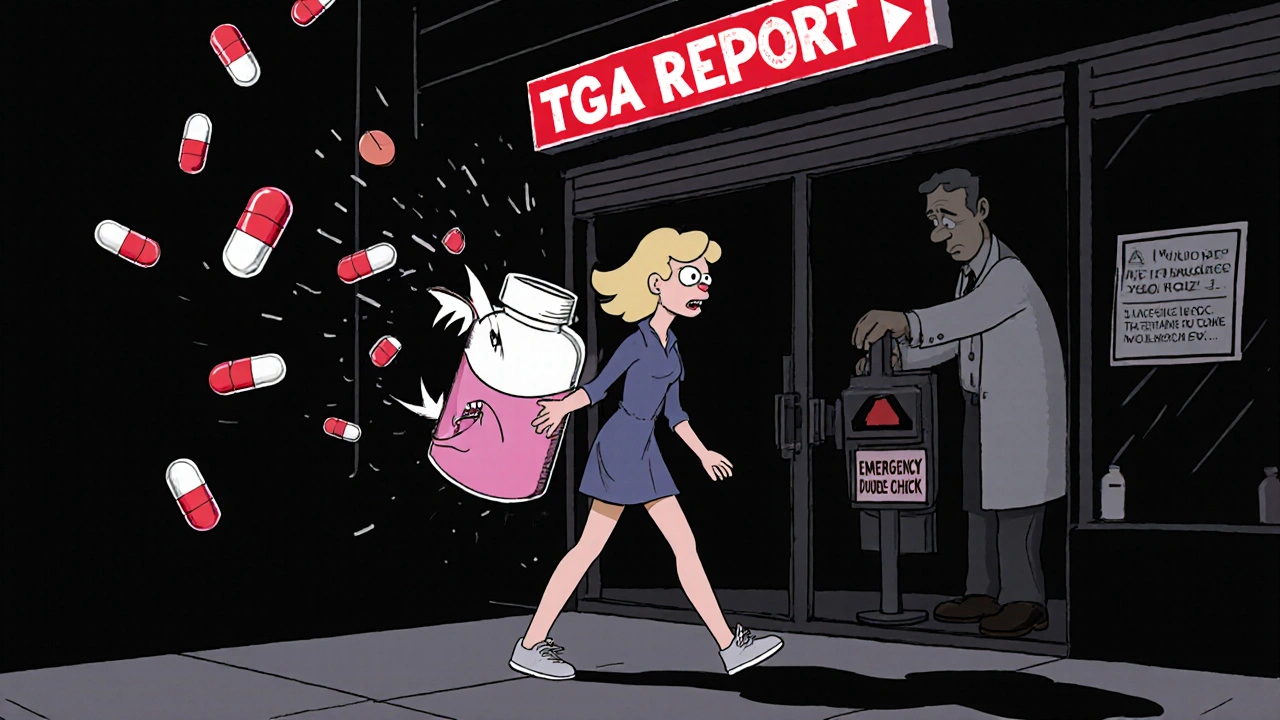
What to Do If You Get the Wrong Medicine
If you realize after leaving the pharmacy that you got the wrong medicine:- Don’t take it.
- Call the pharmacy immediately. Bring it back.
- Notify your doctor. They need to know in case it affected your health.
- Report it to the Therapeutic Goods Administration (TGA) via their website. Your report helps improve safety for everyone.
Real Example: What Happened to Sarah
Sarah, 68, from Toowoomba, was prescribed Warfarin for a blood clot. She’d taken it for years. When she picked up her refill, the pill looked different-smaller, white instead of yellow. She didn’t say anything. She took it. Three days later, she bruised easily and felt dizzy. Her daughter noticed and checked the bottle. The label said Warfarin, but the pill was actually Levothyroxine, a thyroid medication. Sarah had been taking the wrong drug for days. She went back to the pharmacy. They apologized. The pharmacist had confused two similar-looking bottles. Sarah reported it to the TGA. The pharmacy changed their storage system. Sarah now uses her checklist. She takes photos. She asks the three questions. She never walks away without checking.Final Tip: Make It a Habit
You don’t need a fancy app or a printed card. Just remember this: - Know what you’re supposed to get. - Check the label before you leave. - Ask the three questions. - Compare with the old bottle. - Take a photo. Do this every time. Even if you’ve been getting the same medicine for 10 years. Even if the pharmacist knows you by name. Even if you’re in a hurry. Medication errors don’t happen because someone is evil. They happen because systems are complex and people are human. You’re not responsible for fixing the system. But you are responsible for protecting yourself. Your checklist isn’t about distrust. It’s about awareness. It’s about being part of your own care.Do I really need a checklist if the pharmacist is trained?
Yes. Pharmacists are trained, but they work in fast-paced environments with high volumes. Studies show that even the most experienced pharmacists make mistakes-especially with look-alike or sound-alike drugs. A personal checklist adds a layer of protection that no system can replace.
Can I use a printed checklist or should I keep it on my phone?
Either works. A printed checklist you keep in your wallet is great if you’re not tech-savvy. But a digital version on your phone lets you take photos, save notes, and access pill identifiers. Choose what’s easiest for you to use consistently.
What if I’m not sure what the medicine is for?
Ask. Don’t assume. If you’re unsure why you’re taking a medicine, it could mean the prescription was meant for someone else, or there was a mix-up. Your pharmacist is paid to explain this. If they don’t, ask again-or ask your doctor.
Are generic drugs safe to take?
Yes. Generic drugs in Australia must meet strict standards set by the TGA. They contain the same active ingredient as brand-name drugs. But they can look different-different color, shape, or size. Always check the label for the active ingredient name to confirm it’s the same as your previous prescription.
How often do dispensing errors happen in Australia?
One study by the Australian Institute of Health and Welfare found that about 1 in 200 prescriptions filled in community pharmacies contains a dispensing error. Most are minor, but some can be serious. That’s why even small checks matter.
Can I ask the pharmacist to double-check my prescription?
Absolutely. Many pharmacies have a “double-check” policy for high-risk medications like blood thinners, insulin, or opioids. You can ask them to do one. You’re not asking for special treatment-you’re asking for a standard safety step.

David Cusack
November 20, 2025 AT 19:02Let’s be honest-this checklist is the bare minimum. I’ve seen pharmacists hand out pills with labels that read ‘Take 2x daily’ when the script said ‘Take 1x daily’-and they didn’t even blink. You need more than a checklist. You need a witness. A second set of eyes. A legally binding form signed by the pharmacist in triplicate. Otherwise, you’re just trusting a system that’s been broken since 1987.
Willie Doherty
November 20, 2025 AT 20:47While the intent of this checklist is commendable, the methodology lacks empirical grounding. The assertion that asking three questions reduces error rates by 40% is cited without a peer-reviewed source. Furthermore, photographic documentation introduces privacy and data integrity concerns under GDPR and HIPAA frameworks. The recommendation to compare pill appearance is particularly problematic-generic substitution is legal, regulated, and often clinically indistinguishable. This approach risks fostering unnecessary patient anxiety without measurable safety benefit.
Darragh McNulty
November 21, 2025 AT 17:40This is GOLD. 🙌 Seriously, I used to just grab my meds and run-until my grandma almost took someone else’s blood pressure pill. Now I ask the 3 questions every single time. Even if the pharmacist knows me by my first name. Even if I’ve been getting the same thing for 12 years. 📸 I take pics. 🗒️ I write it down. 💬 I say ‘this looks different’ even if I’m scared. You’re not being annoying-you’re being a hero. Keep doing this. The system needs you.
Elaina Cronin
November 23, 2025 AT 05:01I find it deeply concerning that such a fundamental aspect of patient safety is being framed as an individual responsibility rather than a systemic failure. The onus should not rest on the elderly, the disabled, or the linguistically isolated to verify every prescription. This checklist is a band-aid on a hemorrhage. Pharmacies must be held accountable for implementing fail-safes-automated cross-referencing, barcode scanning, mandatory verbal confirmation-not shifting the burden onto vulnerable populations under the guise of empowerment.
Anne Nylander
November 24, 2025 AT 22:51omg yes!! i did this after my uncle got the wrong diabetes pill and almost went into a coma. now i take pics of every bottle, even if it’s the same one. i write down the name and dose on my phone notes. i ask ‘is this what i’m supposed to get?’ and if they look at me weird, i say it again. you’re not weird for asking. you’re smart. and if you’re scared? just say ‘i need to double check with my doctor’-they’ll fix it. you got this 💪❤️
Cooper Long
November 25, 2025 AT 11:23The utility of this checklist is not in question. However, the cultural assumption that patient vigilance compensates for institutional negligence is a distinctly American phenomenon. In nations with centralized pharmaceutical oversight-such as the United Kingdom-the incidence of dispensing errors is significantly lower due to standardized protocols and audit trails. This document, while well-intentioned, reflects a reactive rather than proactive approach to public health.
Sheldon Bazinga
November 26, 2025 AT 23:44lol why are we all acting like pharmacists are babysitters? i’ve been to 3 different pharmacies in 3 states and not once have i gotten the wrong pill. you think the system’s broken? nah. you just lazy. if you can’t remember if your pill is blue or green, maybe you shouldn’t be taking it. also why are you taking pics of your meds? are you building a drug museum? grow up. stop treating yourself like a toddler.
Sandi Moon
November 27, 2025 AT 20:01Of course this checklist works. But only because it’s a distraction. The real story? The TGA’s database is still partially paper-based. The same pharmacists who are ‘trained’ are also being pressured to fill 80 prescriptions per hour. The ‘three questions’? A PR stunt to make you feel safe while the real machinery-controlled substance tracking, AI verification, mandatory second checks-remains underfunded. And let’s not forget: the pharmaceutical corporations lobby against automation because it cuts their profits. This checklist isn’t safety. It’s propaganda. You’re being told to protect yourself… so they don’t have to fix the system.