 Nov, 22 2025
Nov, 22 2025
Why Medication Storage in Shared Spaces Is a Silent Risk
Imagine this: your teenager grabs a painkiller from the bathroom cabinet after a soccer game. Your elderly parent leaves their insulin on the kitchen counter because the fridge is full. A housemate accidentally takes someone else’s blood pressure pill because the bottles look similar. These aren’t rare accidents-they happen every day in shared living spaces. And the consequences? Hospital visits, overdoses, or medications that stop working because they were stored wrong.
Medications aren’t just pills. They’re chemicals that degrade if exposed to heat, moisture, or light. They can be deadly if taken by the wrong person. In shared homes-whether it’s a multi-generational house, an assisted living facility, or a group home-there’s no room for guesswork. The Joint Commission found that between 2020 and 2021, 13% of hospitals got cited for improper medication storage. That’s not a hospital problem. That’s a home problem too.
Lock It Up-No Exceptions
There’s one rule that applies everywhere: medications must be locked away. Not just "put in a drawer." Not just "keep out of reach." Locked. Period.
In professional care homes, 100% of large facilities use locked medication carts or rooms. But in family homes? Only 28% do. That’s a huge gap. A SeniorHelpers survey of 250 families found that 67% had at least one medication-related incident in the past year. Over 40% of those involved kids pulling pills from unsecured cabinets-often the bathroom or kitchen.
Use a locked box. A medicine safe. A cabinet with a child lock. Even a small lockbox from the hardware store works. Don’t rely on "they know better." Kids explore. Seniors get confused. Roommates get careless. Locking isn’t about distrust-it’s about design. Make it hard to accidentally take the wrong thing.
Where to Store: Not the Fridge Door
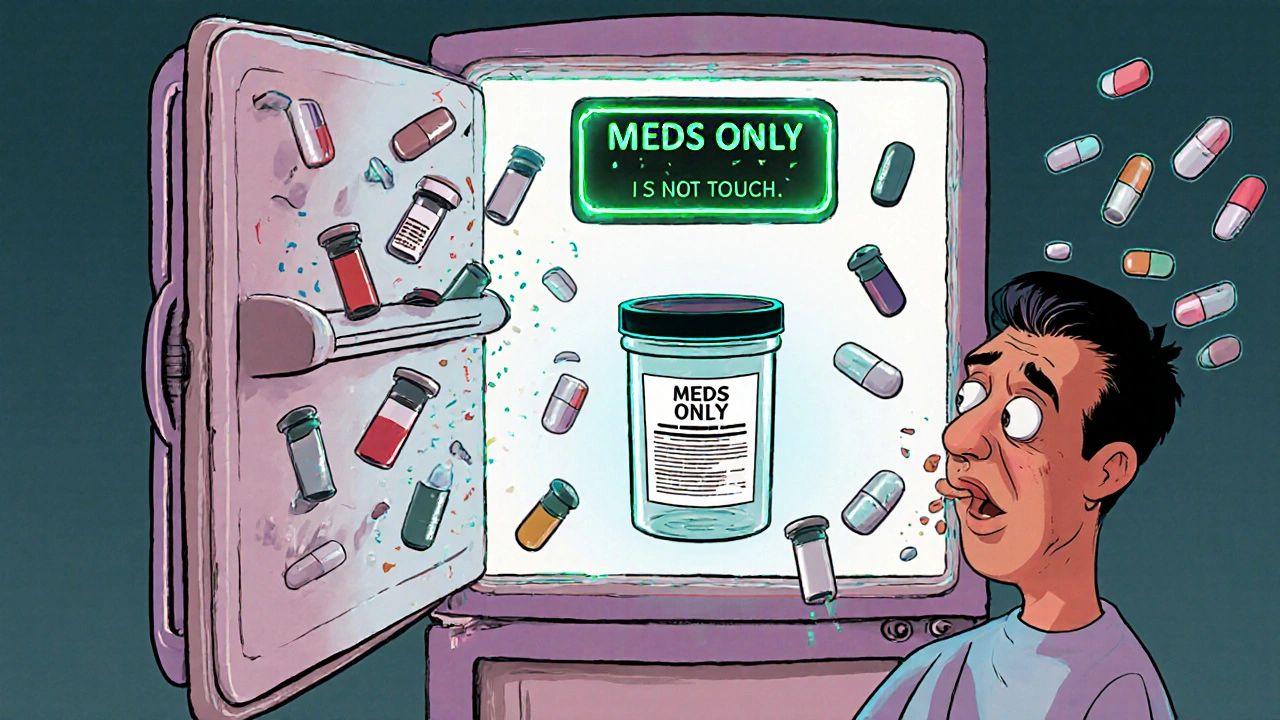
Not all meds need refrigeration, but the ones that do? They need the right spot.
Insulin, some antibiotics, eye drops, and biologics require 36-46°F. The center shelf of your fridge is the only place that stays steady. The door? It swings 10°F or more every time you open it. One caregiver on CareGiverForum shared that her father’s blood sugar went wild after insulin sat on the fridge door for three weeks. The medication was still in the bottle-but it had degraded by over 30%.
Keep food and meds separate. If you must share a fridge, use a sealed, labeled container. Put it on the center shelf. Tape a note: "MEDICATION-DO NOT TOUCH." And never, ever store meds in the freezer unless the label says so. Freezing can destroy some drugs.
Label Everything-Even the Obvious
"My mom’s blood pressure pill" isn’t enough. "Lisinopril 10mg, taken daily at 8 AM, for John Smith" is.
The Joint Commission found that 12% of hospitals got cited for poor labeling. In homes, it’s worse. Bottles get mixed up. Labels wear off. Someone takes a pill because it looks like their own.
Use permanent markers or waterproof labels. Write the person’s full name, the drug name, dosage, and time of day. If it’s a liquid, write the volume. If it’s a pill, write the color and shape. For shared spaces, consider using a pill organizer with clear compartments labeled by day and time. Pre-filled bubble packs from pharmacies are ideal-they cut down confusion and reduce errors.
Separate Controlled Substances
Any medication with a risk of misuse-opioids, benzodiazepines, stimulants-needs extra security. These aren’t just pills. They’re potential targets for theft or abuse.
Store them in a separate locked container, ideally one with an audit trail. Some smart medicine safes now log who opens them and when. In assisted living, staff must sign out each dose. In homes, you don’t need tech-you just need discipline. Keep these meds in a different lockbox than the rest. Only one person should have the key or code. If someone else needs to access them, they must ask, log it, and return it immediately.
Get Rid of the Old Stuff
Old meds are dangerous meds. Expired antibiotics lose potency. Painkillers from five years ago can still be potent enough to kill. The Joint Commission cited 10% of hospitals for expired medications. In homes, it’s even more common.
Do a full cleanup every six months. Check every cabinet, drawer, purse, and nightstand. Look for:
- Pills with changed color or smell
- Liquids that are cloudy or have particles
- Labels with faded or missing info
- Medications no longer prescribed
Don’t flush them. Don’t throw them in the trash. Take them to a pharmacy drop-off or a local drug disposal event. Many police stations and pharmacies offer free, safe disposal. In Brisbane, check with the Queensland Health website for drop-off locations.
Document What’s What
Professional care homes use Medication Administration Records (MARs)-detailed logs that track who took what, when, and if it was given correctly. Most families don’t. But you should.
Even a simple spreadsheet or notebook helps. List each person’s meds: name, dose, time, purpose. Note if it’s taken with food, if it causes drowsiness, or if it interacts with alcohol. Update it when prescriptions change. Share it with anyone who helps with care-your partner, your teen, your visiting nurse.
Why? Because when something goes wrong, you need to know what was taken. And when a doctor asks, "What are they on?"-you won’t have to guess.

Train Everyone Who Lives There
Storage isn’t just about locks and labels. It’s about awareness.
In care homes, staff get 8-12 hours of training. In homes? Nobody gets trained. That’s a problem.
Hold a 20-minute family meeting. Show everyone:
- Where the meds are stored
- Who they belong to
- How to recognize if something looks wrong
- What to do if a pill is missing or taken by accident
Teach kids: "This isn’t candy. Taking someone else’s pill can make you sick-or worse." Teach seniors: "If you can’t read the label, don’t take it. Ask first." Make it normal to check before you take anything.
What’s Changing in 2025
Technology is catching up. Smart medication safes now monitor temperature and humidity. Some even send alerts if the door is opened at 3 a.m. DosePacker rolled out these systems in over 100 facilities in 2024. For families, home medication safes with digital logs are now easier to buy and cheaper than ever.
SeniorHelpers launched a free certification program for family caregivers in April 2025. Over 12,500 people signed up in the first month. It’s not about becoming a nurse. It’s about becoming a safe steward of someone else’s health.
Final Rule: It’s Not a Chore. It’s a Lifesaver.
Managing medication in a shared home isn’t about perfection. It’s about consistency. One locked box. One labeled bottle. One clean-out every six months. One conversation with everyone who lives there.
Every year, over 125,000 Americans end up in the ER because of accidental medication errors in homes. You don’t need a fancy system. You just need to care enough to lock it, label it, and keep it clean.
Start today. Don’t wait for a crisis. Your home, your rules. Make them safe ones.
Can I store all medications in the same locked box?
Yes, but only if they don’t need special conditions. Keep controlled substances (like opioids or sedatives) in a separate lockbox. Also, if you have insulin or other refrigerated meds, store those in a sealed container in the fridge-not in the same box as pills at room temperature. Mixing storage types increases risk.
What if someone refuses to use a locked cabinet?
Explain the risks plainly: "If a child takes your painkiller, they could stop breathing. If your insulin gets warm, it won’t work-and you could end up in the hospital." If they still resist, store their meds in your bedroom or another secure spot. You’re not being controlling-you’re preventing harm. In many cases, people just don’t realize how dangerous unsecured meds can be.
How often should I check expiration dates?
Every six months. Set a reminder for January 1 and July 1. Check each bottle. If the label is faded, the pill looks discolored, or the liquid is cloudy, throw it out. Don’t wait for the printed date-some meds lose potency weeks before expiration. When in doubt, dispose of it.
Is it okay to keep meds in a purse or backpack?
Only if it’s temporary. Purses and backpacks get hot, cold, damp, and jostled. Pills can degrade. Insulin can spoil. If someone needs to carry meds daily, use a small, insulated pill case with a secure lid. Never leave them in a car or on a windowsill. And always return them to the main locked storage at the end of the day.
What’s the best way to dispose of old or unused meds?
Never flush or trash them. Take them to a pharmacy that offers a drug take-back program. In Brisbane, check the Queensland Health website for drop-off locations. Many police stations and community centers also host disposal events. If no options are available, mix pills with coffee grounds or cat litter, seal them in a container, and throw them in the trash-but only as a last resort.

Melvina Zelee
November 24, 2025 AT 04:43steve o'connor
November 25, 2025 AT 14:14ann smith
November 27, 2025 AT 14:12Julie Pulvino
November 27, 2025 AT 16:44Patrick Marsh
November 28, 2025 AT 08:24james lucas
November 28, 2025 AT 15:15Jessica Correa
November 30, 2025 AT 15:14manish chaturvedi
December 2, 2025 AT 08:29Justin Daniel
December 3, 2025 AT 22:54Robin Johnson
December 4, 2025 AT 11:54Latonya Elarms-Radford
December 6, 2025 AT 05:22Mark Williams
December 6, 2025 AT 05:25Daniel Jean-Baptiste
December 8, 2025 AT 04:44Ravi Kumar Gupta
December 8, 2025 AT 05:28Rahul Kanakarajan
December 10, 2025 AT 04:49