 Oct, 1 2025
Oct, 1 2025
Quick Takeaways
- Both intestinal and vaginal infections arise from bacteria, parasites, or yeast that upset the natural balance.
- Common intestinal signs: watery diarrhea, cramping, fever, and nausea.
- Typical vaginal clues: itching, abnormal discharge, burning during urination, or odor.
- When symptoms linger more than a few days, are severe, or include blood, see a health professional.
- Preventive steps include safe food handling, good hygiene, and probiotic‑rich foods.
Understanding why these infections happen and how they feel is the first step toward quick relief and long‑term health. Below we break down the main causes, the tell‑tale symptoms, and practical actions you can take today.
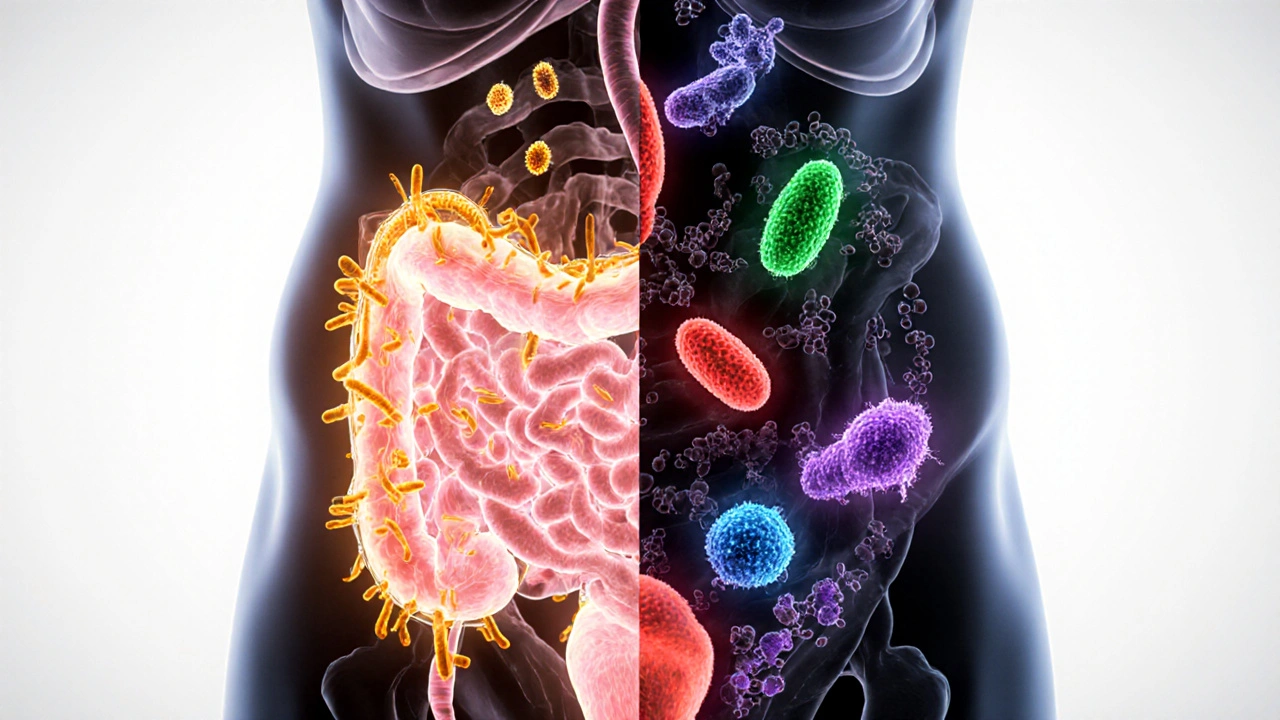
What is an Intestinal infection?
An infection that targets the gastrointestinal tract, disrupting digestion and nutrient absorption. It can be sparked by contaminated food, water, or even an overgrowth of harmful microbes already living in the gut.
What is a Vaginal infection?
A condition in which the natural flora of the vagina is disturbed, allowing pathogenic organisms to multiply. The result is irritation, discharge, and sometimes a lingering odor.
Major Causes of Intestinal Infections
Most gut bugs fall into three categories: bacteria, parasites, and toxins. Below are the most frequent culprits.
- Escherichia coli - especially the Shiga‑toxin producing strains that hitch a ride on undercooked beef or unwashed produce.
- Salmonella - found in raw poultry, eggs, and reptile contact.
- Clostridioides difficile - often blooms after a course of broad‑spectrum antibiotics.
- Giardia lamblia - a protozoan picked up from untreated water or hiking trips.
- Viral agents such as Norovirus - the infamous “cruise‑ship bug”.
Each of these organisms hijacks the gut’s normal processes, leading to inflammation and the classic symptoms listed next.
Typical Intestinal Symptoms
When the gut is under attack you’ll notice one or more of the following:
- Watery or bloody diarrhea (often 3+ loose stools per day)
- Abdominal cramps that come and go
- Nausea or vomiting, especially after meals
- Low‑grade fever (under 38.5°C)
- Loss of appetite and quick‑onset fatigue
If dehydration signs appear - dry mouth, dizziness, or dark urine - it’s time to rehydrate aggressively and consider medical care.

Major Causes of Vaginal Infections
The vagina normally hosts a healthy mix of Lactobacillus species that keep the environment acidic. Disruption can happen for several reasons.
- Bacterial vaginosis (BV) - overgrowth of anaerobic bacteria like Gardnerella vaginalis. Often linked to sexual activity or douching.
- Yeast infection (Candidiasis) - proliferation of Candida albicans. Triggered by antibiotics, high‑sugar diet, or tight clothing.
- Sexually transmitted infections (STIs) - such as Trichomonas vaginalis or chlamydia, which directly invade the mucosa.
- Hormonal shifts during pregnancy, menopause, or birth control changes.
- Foreign objects (e.g., forgotten tampons) creating a moist, anaerobic pocket.
Understanding the root cause helps pick the right treatment - antibiotic, antifungal, or probiotic.
Typical Vaginal Symptoms
Vaginal infections share a handful of red‑flag signs:
- Itching or burning that intensifies after intercourse
- Unusual discharge - white and clumpy (yeast), thin and gray (BV), or frothy yellow‑green (Trichomonas)
- Odor ranging from “cheesy” (BV) to “fishy” (Trichomonas)
- Soreness during urination or after wiping
- Occasional spotting or mild bleeding
When the discharge is thick, odorless, and accompanied by severe pain, it could signal a more serious condition and warrants prompt evaluation.
How to Differentiate Between Intestinal and Vaginal Issues
Because some symptoms overlap - mainly abdominal discomfort and changes in bowel movements - a quick self‑check can point you in the right direction.
| Feature | Intestinal Infection | Vaginal Infection |
|---|---|---|
| Primary discomfort | Cramping around the belly | Itching/burning around vulva |
| Discharge | Mostly stool‑related (diarrhea) | Vaginal fluid changes |
| Odor | Usually none unless severe infection | Fishy or yeasty smell |
| Fever | Common, especially with bacterial cause | Rare, unless systemic STI |
| Trigger | Contaminated food, water, antibiotics | Antibiotics, hormonal shifts, sexual activity |
When you notice both gastrointestinal and vaginal symptoms together, consider a shared cause such as antibiotics wiping out good bacteria, which can invite both C.difficile and yeast overgrowth.
When to Seek Professional Care
Most mild infections clear up in a few days with home care, but these warning signs merit a doctor’s visit:
- Diarrhea lasting longer than three days, especially with blood.
- High fever (above 38.5°C) or persistent chills.
- Severe abdominal pain that does not improve.
- Vaginal discharge that is green, yellow, or has a strong odor for more than two days.
- Painful urination combined with vaginal symptoms - could be a urinary tract infection.
- Recurring infections (more than two episodes in six months).
Early diagnosis often involves stool tests, vaginal swabs, or even a simple urine dip to rule out mixed infections.
Prevention Tips You Can Start Today
Keeping the gut and vagina in balance isn’t rocket science. Here are evidence‑backed habits that work.
- Food safety first: wash fruits and veggies, cook meats to proper internal temperatures, and avoid cross‑contamination.
- Stay hydrated: adequate water supports a healthy mucosal barrier in both the gut and vaginal tract.
- Probiotic power: fermented foods like yogurt, kefir, and sauerkraut supply live cultures that compete with pathogens.
- Smart antibiotic use: only take them when prescribed, and follow the full course to prevent resistant strains.
- Gentle hygiene: use unscented soap, avoid douching, and wear breathable cotton underwear.
- Safe sex practices: condoms reduce STI risk and lower the chance of bacterial imbalance.
- Regular check‑ups: annual pelvic exams can catch early signs before they flare up.
By weaving these habits into daily life, you reduce the odds of both intestinal infections and vaginal mishaps.

Frequently Asked Questions
Can I treat a vaginal infection with over‑the‑counter products?
Mild yeast infections often respond to OTC creams containing clotrimazole or miconazole. However, bacterial vaginosis and STIs require prescription medication, so a clinician visit is advisable if symptoms persist after a few days.
Is it safe to take probiotics while I have an intestinal infection?
Yes, most studies show that probiotics can shorten the duration of antibiotic‑associated diarrhea and may help restore gut flora after a bacterial infection. Choose strains like Lactobacillus rhamnosus GG or Saccharomyces boulardii.
How long does it usually take for symptoms to improve?
For most food‑borne bacteria, 24‑48hours of proper hydration and rest bring noticeable relief. Yeast infections often improve within three days of using an antifungal cream. Persistent or worsening signs after 72hours merit a medical review.
Can I get a vaginal infection from a toilet seat?
The risk is extremely low. Most vaginal infections stem from internal flora changes rather than surface contact. Good hygiene, however, still helps prevent secondary irritation.
What is the link between antibiotics and yeast infections?
Broad‑spectrum antibiotics kill both harmful and beneficial bacteria, including Lactobacillus that keep Candida in check. The resulting imbalance allows yeast to multiply, leading to itching and discharge.

namrata srivastava
October 1, 2025 AT 16:46The pathophysiology of intestinal and vaginal dysbiosis is underpinned by a perturbation of the symbiotic microbial consortium, precipitating a cascade of inflammatory mediators and epithelial barrier compromise. Contemporary gastroenterological literature delineates the etiological nexus between antimicrobial stewardship lapses and opportunistic overgrowth of pathogenic taxa such as Clostridioides difficile, which exploits the vacated niche. Analogously, vaginal eubiosis is contingent upon Lactobacillus-dominant acidification, the erosion of which augments susceptibility to Gardnerella‑induced bacterial vaginosis and Candida proliferation. The clinical rubric necessitates a bifurcated diagnostic algorithm integrating stool cultures, PCR panels, and vaginal swab microscopy to differentiate etiologies with precision. Therapeutic stratagems should be predicated upon targeted antimicrobial agents coupled with adjunctive probiotic reconstitution to restore homeostatic equilibrium.
Priyanka arya
October 17, 2025 AT 10:13Wow, you think all this is just about germs? 👀 Maybe the pharma giants are hiding the real cure and feeding us endless cycles of antibiotics so they can keep the shortages coming! 🌐💊 And don't even get me started on how the “clean water” narrative is a cover‑up for the mineral‑rich streams they’re secretly dumping into our tap. 😂 Stay woke, folks, the truth is out there!
Alan Clark
November 2, 2025 AT 02:40Honestly, this stuff can feel overwhelming but just remember your body’s pretty good at bouncing back if you give it the right fuel and rest. Drink plenty of water, munch on some probiotic‑rich yoghurt, and if the cramps keep dragging on, give your doc a ring. It’s all about keeping that gut‑vaginal balance in check, you’ll be fine.
Mark Anderson
November 17, 2025 AT 20:08Right on, mate! 🌟 Adding a splash of colorful veggies and a dash of fermented kimchi can turn the tide in your favor. Keep the mindset upbeat and the microbes will thank you-trust the process and stay positive!
Shouvik Mukherjee
December 3, 2025 AT 13:35Hey everyone, let’s remember that health is a shared journey across cultures. Simple habits like washing hands with mild soap, choosing breathable cotton undergarments, and staying hydrated are universal. Supporting each other with kind advice creates a stronger community for everyone.
Ben Hooper
December 19, 2025 AT 07:02What about the role of prebiotic fibers in preventing these infections
Marjory Beatriz Barbosa Honório
January 4, 2026 AT 00:30It’s amazing how a few mindful choices can make a huge difference in our wellbeing. Staying hydrated, eating fermented foods, and practicing gentle hygiene are simple steps that empower us to keep both gut and vaginas thriving. Let’s keep uplifting each other with these practical tips!
G.Pritiranjan Das
January 19, 2026 AT 17:57Remember, consistency beats intensity every time.
Karen Wolsey
February 4, 2026 AT 11:24Oh sure, because ignoring basic hygiene and then blaming “bad luck” is the new trend, right? 🙄 If you skip the simple stuff, surprise you’ll end up dealing with infection.
Trinity 13
February 20, 2026 AT 04:51When we contemplate the intricate symbiosis between microbial consortia and human physiology, we are forced to confront a cascade of philosophical considerations that extend beyond mere clinical symptomatology. The gut, often dubbed the “second brain,” orchestrates not only digestion but also immune modulation, neurotransmitter synthesis, and even mood regulation, thereby weaving a tapestry of interdependence that defies reductionist paradigms. Likewise, the vaginal ecosystem, anchored by Lactobacillus dominance, serves as a sentinel against pathogenic invasion, maintaining an acidic milieu that is both protective and indicative of holistic health. Disruption of these finely tuned habitats-whether through indiscriminate antibiotic use, dietary monotony, or environmental toxins-can precipitate a state of dysbiosis that reverberates through the body’s intricate feedback loops. It is tempting, however, to attribute such disturbances solely to microbial misbehavior, ignoring the sociocultural practices that shape our exposure to risk factors. For instance, the prevalence of tight, synthetic clothing in modern wardrobes not only traps moisture but also creates anaerobic pockets conducive to fungal overgrowth. Moreover, the paradox of sanitation lies in its dual capacity to shield us from pathogens while simultaneously stripping away beneficial microbial exposures that educate our immune system. The concept of “hygiene hypothesis” encapsulates this tension, urging a re‑evaluation of what constitutes true cleanliness.
In pragmatic terms, the remedy is not a return to primitive living but rather an integration of evidence‑based practices that honor both microbial diversity and personal autonomy. Regular consumption of fermented foods-such as kefir, sauerkraut, and miso-supplies live cultures that compete with opportunistic pathogens, reinforcing the natural defenses of the gut and vagina alike. Hydration, often overlooked, underwrites mucosal integrity, ensuring that epithelial barriers remain resilient. Gentle, unscented cleansing rituals safeguard the delicate pH balance without provoking irritation or eliminating beneficial flora. Finally, a judicious approach to pharmaceuticals, reserving antibiotics for confirmed bacterial infections and adhering strictly to prescribed courses, mitigates collateral damage to commensal populations. Such holistic stewardship transforms illness prevention into an act of self‑respect and communal responsibility. By weaving these threads into the fabric of daily life, we craft a resilient tapestry of health that transcends the episodic flare‑ups of infection, inviting a continual dialogue between body, microbiome, and the world we inhabit.