 Nov, 21 2025
Nov, 21 2025
Why One Size Doesn’t Fit All in Medication Dosing
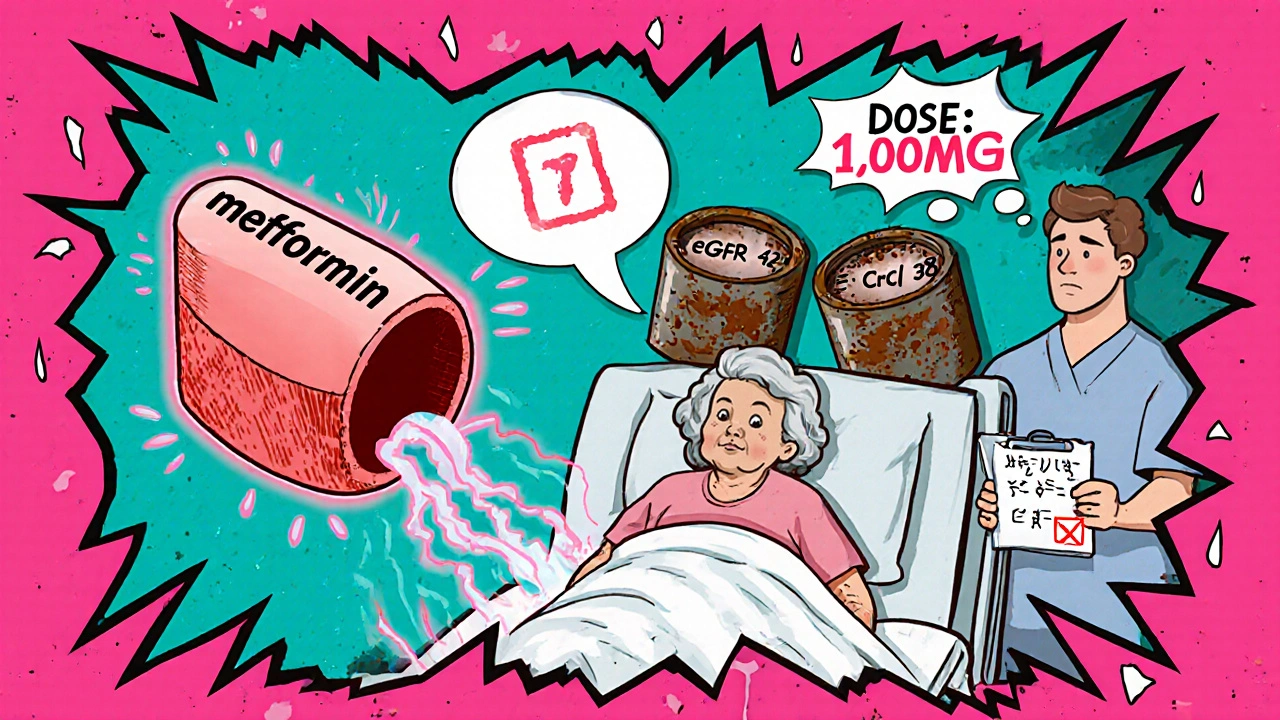
Take a 78-year-old woman with type 2 diabetes and stage 3 kidney disease. She’s prescribed metformin at 1000 mg twice daily-exactly what her doctor saw on the standard prescription chart. But her kidneys aren’t clearing the drug like they did when she was 40. Within months, she ends up in the hospital with lactic acidosis. This isn’t rare. It’s preventable. And it happens because dosing rules for older adults, people with low or high body weight, or those with kidney problems aren’t just suggestions-they’re life-or-death calculations.
Medications don’t act the same in every body. Your age, how much you weigh, and how well your kidneys work change how drugs move through you, how long they stay, and how strong their effect becomes. A dose that’s safe for a 30-year-old athlete might be toxic for a 70-year-old with reduced kidney function. That’s why adjusting medication doses isn’t optional. It’s basic safety.
How Kidney Function Changes Everything
Your kidneys filter about 120 to 150 quarts of blood every day. If they’re working at full capacity, they remove waste and excess drugs efficiently. But if your kidney function drops-even slightly-many medications build up in your blood. That’s when side effects turn dangerous.
Doctors don’t just look at your serum creatinine level. They use formulas to estimate how well your kidneys are filtering, called glomerular filtration rate (eGFR). The most accurate formula today is the CKD-EPI equation, which takes into account your age, sex, race, and creatinine level. It’s now used in most labs to stage chronic kidney disease (CKD):
- Stage 1: eGFR ≥90 (normal, but with signs of damage)
- Stage 2: eGFR 60-89 (mild reduction)
- Stage 3a: eGFR 45-59 (mild to moderate)
- Stage 3b: eGFR 30-44 (moderate to severe)
- Stage 4: eGFR 15-29 (severe)
- Stage 5: eGFR <15 (kidney failure)
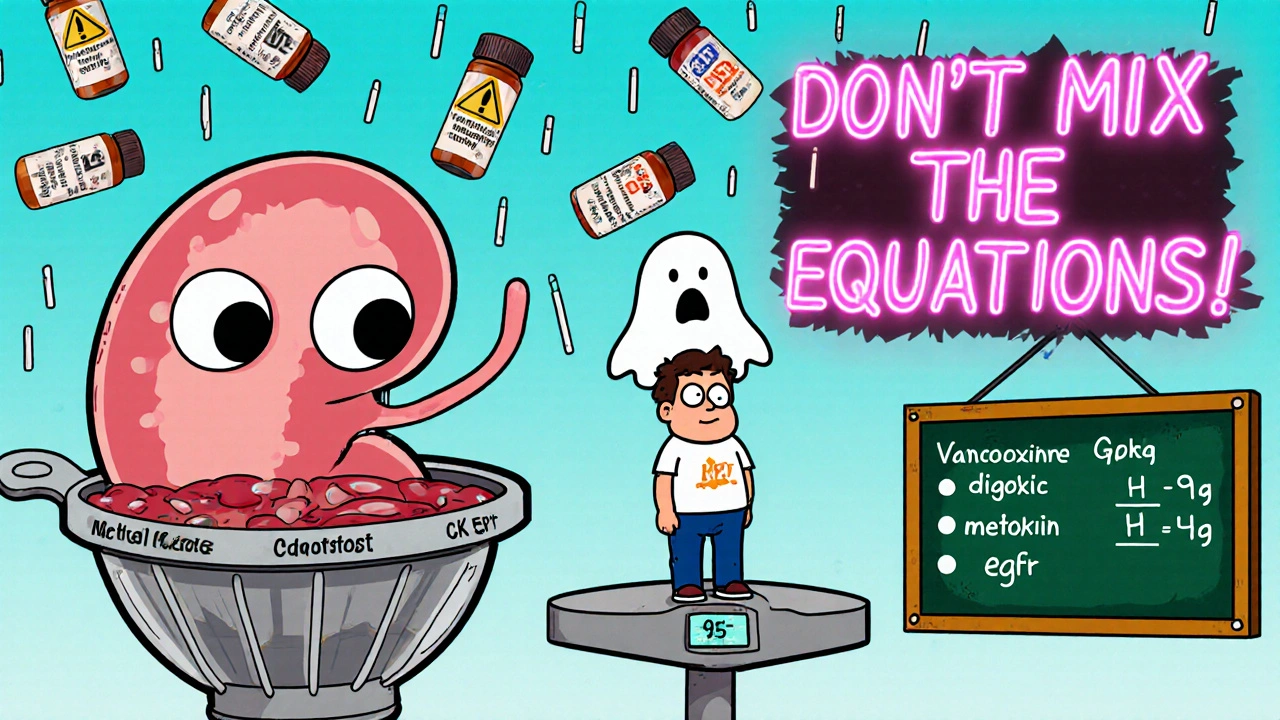
But here’s the catch: while CKD-EPI is great for diagnosing kidney disease, it’s not always the best for dosing medications. Many drug labels still rely on the older Cockcroft-Gault equation, which estimates creatinine clearance (CrCl) using your age, weight, and sex. Why? Because most drug studies in the 1980s and 90s used CrCl. So even today, if you’re on vancomycin, digoxin, or many antibiotics, your dose depends on CrCl-not eGFR.
That means your doctor might need to calculate two numbers: one for kidney staging (eGFR), and another for drug dosing (CrCl). Confusing? Yes. But skipping either one can lead to underdosing or overdose.
Weight Matters More Than You Think
Let’s say you’re overweight. Does that mean you need more of a drug? Not always. Some drugs spread out in fat tissue. Others stay in water. That’s why using your actual body weight can be misleading.
For people with a BMI over 30, doctors use adjusted body weight instead. The formula is simple: Adjusted weight = Ideal body weight + 0.4 × (actual weight − ideal weight).
What’s ideal body weight? For men: 50 kg + 2.3 kg for every inch over 5 feet. For women: 45.5 kg + 2.3 kg for every inch over 5 feet. So a 6-foot-tall man who weighs 110 kg has an ideal weight of 77.6 kg. His adjusted weight? Around 90 kg-not 110 kg. If you used his full weight to calculate kidney clearance, you’d overestimate his kidney function by 15-20%. That could mean giving him too much of a drug like gentamicin or insulin.
On the flip side, if you’re underweight (BMI under 18.5), Cockcroft-Gault can overestimate your kidney function by up to 25%. That’s why in elderly or frail patients, even if their creatinine looks normal, their actual kidney function might be much lower. Dosing based on real kidney function-not just lab numbers-is critical.
Age Isn’t Just a Number
As you get older, your body changes. Muscle mass drops. Fat increases. Blood flow to your kidneys slows. All of this affects how drugs are absorbed, distributed, and cleared.
Studies show that by age 70, kidney function drops by about 1% per year. That means a 75-year-old might have only 60% of the kidney function they had at 30-even if their creatinine is “normal.” That’s why many drugs need lower doses in older adults, even without a formal kidney disease diagnosis.
Take warfarin. It’s thinning the blood. Too much, and you bleed. Too little, and you get a clot. In older adults, even small changes in dose can tip the balance. The same goes for benzodiazepines, opioids, and antipsychotics. These drugs stick around longer in elderly bodies. A dose that was fine at 50 becomes risky at 80.
And it’s not just kidneys. Your liver slows down too. Many drugs are broken down by the liver before they reach the bloodstream. That’s called first-pass metabolism. As you age, that process weakens. So drugs like statins or certain antidepressants can build up faster than expected.
What Drugs Need the Most Attention?
Not every medication needs adjustment. But some are high-risk. Here are the top categories where dosing errors are most common:
- Antibiotics: Vancomycin, aminoglycosides, penicillins. These are cleared mostly by the kidneys. Too high? Kidney damage. Too low? Treatment fails.
- Diabetes drugs: Metformin, SGLT2 inhibitors, insulin. Metformin is banned if eGFR is below 30. SGLT2 inhibitors like dapagliflozin are stopped if eGFR drops below 45.
- Heart medications: Digoxin, amiodarone, beta-blockers. These have narrow safety windows. Even small changes in kidney function can cause toxicity.
- Painkillers: NSAIDs like ibuprofen or naproxen. They reduce blood flow to the kidneys. In someone with CKD, they can cause sudden kidney failure.
- Anticonvulsants: Gabapentin, pregabalin. Almost entirely cleared by kidneys. Dose must drop as eGFR falls.
According to a 2022 survey by the American Society of Health-System Pharmacists, 68% of pharmacists see inappropriate renal dosing at least once a week. Antibiotics were the most common error (32%), followed by heart meds (28%) and diabetes drugs (22%).
How to Get It Right: A Practical Guide
Here’s how to avoid common mistakes:
- Know which equation to use: For drug dosing, use Cockcroft-Gault (CrCl). For staging kidney disease, use CKD-EPI (eGFR). Don’t mix them up.
- Use adjusted weight for obesity: If BMI >30, calculate adjusted body weight before plugging into Cockcroft-Gault.
- Check the drug label: Every FDA-approved drug has a renal dosing section. Look for “dose adjustment based on CrCl” or “not recommended if eGFR <30.”
- Don’t assume normal creatinine = normal kidneys: In elderly or frail patients, creatinine can be low even if kidneys are failing. Always calculate CrCl.
- Use clinical decision tools: Hospitals with automated alerts reduce dosing errors by nearly half. If your doctor doesn’t use them, ask why.
For example: A 72-year-old woman with type 2 diabetes, weight 65 kg, serum creatinine 1.4 mg/dL. Her eGFR (CKD-EPI) is 42 mL/min/1.73m²-Stage 3b. Her CrCl (Cockcroft-Gault) is 38 mL/min. She’s on metformin. Standard dose: 1000 mg twice daily. But FDA guidelines say: max 500 mg daily if CrCl is 30-45. That’s the difference between safety and hospitalization.
What’s Changing in 2025?
Technology is catching up. The FDA’s 2023 draft guidance pushes for individualized dosing-not just based on age or weight, but on real-time monitoring. Pilot programs are testing wearable sensors that estimate kidney function continuously. Imagine a patch that tells your phone your CrCl every hour. That’s coming by 2026.
Also, a new standardized renal dosing database is launching in mid-2025, backed by the American Society of Nephrology and the American Society of Health-System Pharmacists. Right now, you’ll find five different dosing recommendations for the same drug across five different sources. That’s dangerous. This new database will fix that.
And AI is stepping in. NIH is funding $50 million to build algorithms that factor in genetics, body composition, and kidney function to predict the perfect dose. This isn’t sci-fi-it’s happening in 15 major U.S. hospitals by late 2024.
What to Do If You’re on Multiple Medications
If you’re over 65, have diabetes, high blood pressure, or kidney disease, and you take more than three medications, ask your pharmacist or doctor:
- “Which of my meds need a dose change based on my kidney function?”
- “Can you check my creatinine clearance, not just my creatinine level?”
- “Is my dose based on actual weight or adjusted weight?”
- “Has this dose been reviewed since my last kidney test?”
Don’t wait for a problem to happen. A simple blood test and a quick calculation can prevent a trip to the ER. And if your doctor doesn’t know the difference between eGFR and CrCl, find someone who does.
Final Thought: Safety Is a Process, Not a Guess
Medication dosing isn’t magic. It’s math. And it’s personal. What works for your neighbor might hurt you. Your body is unique. Your kidneys are unique. Your weight and age? They matter.
Don’t let a generic prescription be your only guide. Ask questions. Know your numbers. And make sure your care team is using the right formulas-not just the easiest ones.

Katy Bell
November 22, 2025 AT 05:14So many people don’t realize that a 'normal' creatinine level in an elderly person is basically a lie. My grandma’s was always 'fine' until she almost died from metformin buildup. They didn’t even check CrCl. Scary stuff.
shreyas yashas
November 24, 2025 AT 02:47As someone who grew up watching my dad juggle 8 meds after his kidney transplant, this hits hard. I used to think doctors just knew this stuff. Turns out, they’re often winging it with outdated charts. Glad someone finally laid it out like this.
Suresh Ramaiyan
November 25, 2025 AT 12:20It’s funny how we treat medicine like it’s one-size-fits-all when we know our bodies are all so different. My cousin’s 85-year-old aunt got the same insulin dose as her 40-year-old son. She ended up in a coma. The system isn’t broken-it was never built for people like her.
Ragini Sharma
November 26, 2025 AT 10:22ok but like… why do we even have 2 diff formulas? like why not just pick one?? crcl or egfr?? why make doctors do extra math?? also i think i spelled glomerular wrong lol
Adrian Rios
November 28, 2025 AT 09:29Let’s be real-this isn’t just about kidney function or weight. It’s about how healthcare commodifies human bodies. We reduce people to lab values because it’s faster, cheaper, and easier for the system. But when you’re the 78-year-old woman on metformin who ends up in ICU because no one bothered to calculate CrCl, you realize this isn’t just a ‘clinical oversight’-it’s a moral failure. And the fact that we’re still using Cockcroft-Gault because ‘that’s what the studies used’? That’s not science. That’s institutional inertia. We’re not just underdosing or overdosing-we’re under-valuing lives. And AI won’t fix that unless we demand it to be trained on equity, not just data. The new FDA guidance? Good start. But without enforcement, it’s just another PowerPoint slide. Real change means auditing every hospital’s dosing protocols, not just updating drug labels.
Lisa Detanna
November 28, 2025 AT 23:53As a nurse in a rural ER, I see this every week. A 70-year-old comes in with confusion, and the chart says ‘normal creatinine.’ But their CrCl is 28. They’re on gabapentin. No dose adjustment. They almost died. We need mandatory renal dosing training for all prescribers-no exceptions. This isn’t niche. It’s everywhere.
John Mackaill
November 30, 2025 AT 22:47My GP still uses eGFR for everything. I had to print out the FDA’s dosing guidelines and hand them to him. He said, ‘I’ve never been taught CrCl.’ That’s not acceptable. This is basic pharmacology. We need to teach this in med school-not as an elective, but as core.
Matthew Mahar
December 1, 2025 AT 03:47Wait so adjusted weight is like… if you’re fat you get less drug? That seems backwards. I thought more weight = more drug? Confused. Also typo in the formula? I think it’s 0.4 times the difference, not 0.4 x actual minus ideal? Or am I wrong?
Richard Wöhrl
December 1, 2025 AT 22:23Just checked my mom’s chart-she’s on digoxin, CrCl 34, still on 0.125 mg daily. That’s the upper limit. I called the pharmacy. They said they flagged it but the doctor overruled it. I’m going back tomorrow with this post. This isn’t just knowledge-it’s a weapon.
Casper van Hoof
December 3, 2025 AT 11:49The philosophical underpinning of this issue lies in the epistemological asymmetry between biomedical reductionism and embodied subjectivity. While mathematical models provide operational utility, they fail to account for the phenomenological reality of aging as a lived, temporal process. The algorithmic governance of pharmacotherapy, therefore, constitutes a form of technocratic alienation.
Demi-Louise Brown
December 4, 2025 AT 22:19Thank you for this detailed and necessary overview. I’ve shared it with my entire care team. Every provider should be required to read this before prescribing. Safety isn’t optional. It’s non-negotiable.