 Nov, 26 2025
Nov, 26 2025
Psychiatric Medication Interaction Checker
Interaction Analysis
Always consult your doctor or pharmacist before changing any medications. This tool provides information only.
When you’re taking more than one psychiatric medication, it’s not just about how each drug works alone-it’s about how they react together. What seems like a logical combination to a doctor-say, an SSRI for depression and an antipsychotic for anxiety-can turn dangerous if the drugs clash inside your body. These aren’t rare accidents. About 30 to 50% of adverse drug events in psychiatric care come from interactions between medications. And many of them happen in the first few days after a new drug is added.
How These Interactions Actually Happen
Psychiatric drugs don’t float around in your system randomly. They target specific brain chemicals: serotonin, norepinephrine, and dopamine. Each class of medication affects these chemicals differently. For example, SSRIs like fluoxetine or sertraline boost serotonin. SNRIs like venlafaxine raise both serotonin and norepinephrine. Antipsychotics like risperidone block dopamine. When you mix them, you’re not just adding effects-you’re creating unpredictable surges or blockades. The biggest danger comes from too much serotonin. That’s called serotonin syndrome. It can start with mild symptoms like shivering, diarrhea, or restlessness-but it can quickly turn into high fever, seizures, irregular heartbeat, and even death. The risk skyrockets when you combine an SSRI or SNRI with an MAO inhibitor like phenelzine or tranylcypromine. These MAOIs stop your body from breaking down serotonin, so when you add a drug that pumps more serotonin into your brain, it floods the system. There’s no safe middle ground here. Even a small dose of an SSRI added to an MAOI can trigger this reaction. Another major risk comes from drugs that slow down your liver’s ability to process other medications. This is called enzyme inhibition. Fluvoxamine, an SSRI, is one of the strongest inhibitors of CYP enzymes-especially CYP1A2, CYP2C19, and CYP3A4. That means if you’re taking fluvoxamine and also use a drug like clozapine, carbamazepine, or even some common painkillers, your body can’t clear those drugs fast enough. Levels build up, and toxicity follows. One study showed that adding fluvoxamine to clozapine increased clozapine blood levels by over 300% in some patients.High-Risk Combinations You Need to Know
Some combinations are so dangerous they’re practically forbidden unless under strict supervision. Here are the most critical ones:- SSRIs + MAO inhibitors: This is the classic serotonin syndrome trap. Even after stopping an MAOI, you need a 14-day washout period before starting an SSRI. The reverse is true too-wait at least 5 weeks after stopping fluoxetine before starting an MAOI because fluoxetine lingers in your system for weeks.
- TCAs + antihistamines or anticholinergics: Tricyclic antidepressants like amitriptyline already cause dry mouth, constipation, and blurred vision. Add diphenhydramine (Benadryl), oxybutynin, or even some sleep aids, and those side effects multiply. You risk urinary retention, confusion, fast heart rate, and dangerous drops in blood pressure.
- Lithium + NSAIDs or diuretics: Lithium has a very narrow window between effective and toxic. A normal dose can become deadly if your kidneys can’t clear it. NSAIDs like ibuprofen or naproxen reduce kidney blood flow, causing lithium levels to spike by 25-50%. Even a few days of regular painkiller use can push you into toxicity. Symptoms? Tremors, nausea, confusion, and seizures.
- Antipsychotics + alcohol or benzodiazepines: Both depress the central nervous system. Combine them with quetiapine, olanzapine, or risperidone, and you’re looking at extreme drowsiness, slowed breathing, and a higher chance of falling or choking. This combo is especially risky in older adults.
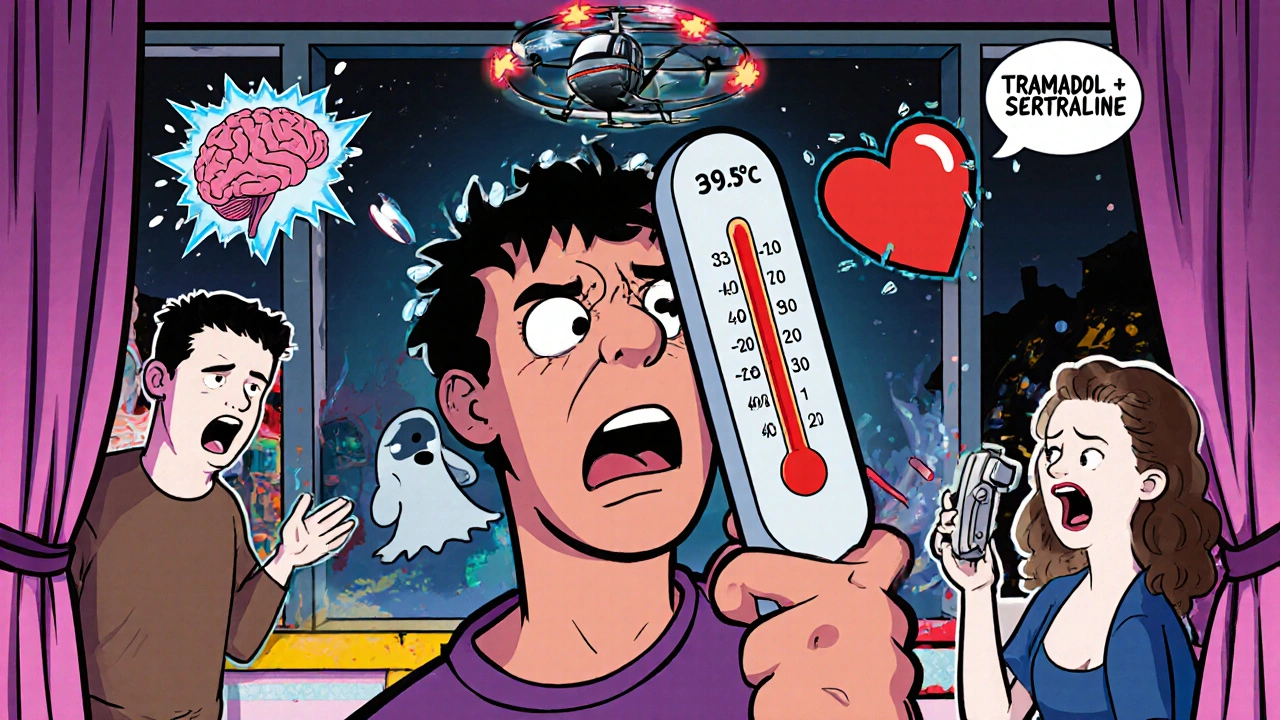
- SSRIs/SNRIs + tramadol or meperidine: These opioids also increase serotonin. When paired with antidepressants, they raise serotonin syndrome risk even without an MAOI. Tramadol is often overlooked because it’s seen as a "mild" painkiller-but it’s one of the most common triggers of serotonin syndrome in combination therapy.
Why New Combinations Are the Most Dangerous
The biggest risk isn’t long-term use-it’s starting something new. When a doctor adds a second or third medication, the body hasn’t adjusted yet. That first dose is when things go wrong. That’s why experts recommend first-dose monitoring: watch the patient for at least 2 to 4 hours after giving a new interacting drug. Look for early signs: agitation, sweating, rapid heartbeat, or muscle stiffness. If those show up, don’t wait. Call for help. Many patients don’t realize how quickly this can escalate. One case from Brisbane in 2024 involved a 58-year-old man who started sertraline for depression and was given tramadol for back pain two days later. He didn’t feel "bad"-just more tired than usual. By day four, he was confused, sweating heavily, and his temperature hit 39.5°C. He ended up in intensive care. His doctors later realized the combination had triggered serotonin syndrome. He survived, but only because his wife noticed the change fast.
What Makes Some Drugs Safer Than Others
Not all psychiatric drugs are created equal when it comes to interactions. Some are "cleaner"-they don’t interfere much with liver enzymes or neurotransmitter systems. For example:- Sertraline and citalopram are SSRIs with low interaction potential. They’re often preferred when someone’s already on multiple meds.
- Vilazodone affects serotonin strongly but doesn’t touch the liver enzymes much, making it safer for people on other drugs.
- Quetiapine has fewer enzyme interactions than other antipsychotics like risperidone or aripiprazole.
- Mirtazapine doesn’t inhibit CYP enzymes and has minimal serotonin effects, so it’s often used as a safer alternative in complex cases.
Monitoring: The Lifeline in Polypharmacy
If you’re on multiple psychiatric drugs, you need more than just monthly check-ins. You need a plan. Here’s what real-world monitoring looks like:- Lithium: Blood levels checked every 3-6 months, or immediately after starting a new drug like an NSAID or diuretic. Safe range is 0.6-1.0 mmol/L. Anything above 1.2 is dangerous.
- Clozapine: Weekly blood tests for the first 6 months to catch agranulocytosis-a rare but deadly drop in white blood cells.
- Valproate: Liver function tests every 3 months. It can cause silent liver damage.
- SSRIs + Warfarin: INR checked weekly for the first month. SSRIs can increase warfarin’s effect, raising bleeding risk.
- Antipsychotics: Use the AIMS scale every 3 months to check for tardive dyskinesia-uncontrollable facial or limb movements that can become permanent.
What You Can Do to Stay Safe
You don’t have to be a doctor to protect yourself. Here’s what works:- Keep a complete list of every medication you take-prescription, over-the-counter, supplements, even herbal teas. Include doses and why you’re taking them.
- Ask your pharmacist every time a new drug is prescribed: "Will this interact with anything else I’m taking?" Pharmacists are trained to spot these clashes.
- Don’t start new meds without telling your psychiatrist. Even something as simple as St. John’s Wort or CBD oil can trigger dangerous interactions.
- Know the warning signs of serotonin syndrome: agitation, sweating, rapid pulse, muscle rigidity, high temperature. If you feel like you’re "melting" from the inside, seek help immediately.
- Use digital tools. Some apps now alert you when a new prescription might clash with your current list. Hospitals in Australia are starting to use these systems-they’ve cut serious interaction events by 37%.
What’s Changing Now
The field is moving fast. In 2022, the Clinical Pharmacogenetics Implementation Consortium updated guidelines for testing genes like CYP2D6 and CYP2C19. These genes control how your body breaks down antidepressants. If you’re a slow metabolizer, even a normal dose of fluoxetine could build up to toxic levels. Genetic testing isn’t routine yet-but more psychiatrists are starting to use it, especially for patients who’ve had bad reactions before. Newer drugs like cariprazine and brexanolone are being studied for interactions, and AI models are being tested to predict individual risk based on your genetics, age, kidney function, and current meds. These won’t replace doctors-but they’ll help them make smarter choices.Final Thought: It’s Not About Avoiding Meds-It’s About Managing Them Wisely
Psychiatric medications save lives. But they’re not harmless. The danger isn’t in taking more than one-it’s in taking the wrong combination without knowing how they’ll behave together. The best outcomes come not from avoiding treatment, but from treating with awareness. If you’re on multiple psychiatric drugs, make sure your care team is watching closely, testing regularly, and listening when you say something doesn’t feel right. Your brain deserves precision-not guesswork.Can I take over-the-counter meds with my psychiatric drugs?
Some OTC drugs can be dangerous. Cold medicines with dextromethorphan, painkillers like ibuprofen or naproxen, and even antihistamines like Benadryl can interact with antidepressants, antipsychotics, or lithium. Always check with your pharmacist before taking anything new-even if it’s sold without a prescription.
Is serotonin syndrome always obvious?
No. Early symptoms like restlessness, sweating, or mild tremors are often mistaken for anxiety or side effects. By the time fever or seizures appear, it’s already severe. If you start a new drug and feel "off" within days-especially if you’re on an SSRI, SNRI, or MAOI-don’t wait. Seek medical help immediately.
How long should I wait between stopping one psychiatric drug and starting another?
It depends on the drug. For most SSRIs, wait 1-2 weeks. But fluoxetine stays in your system for up to 5 weeks, so you must wait that long before starting an MAOI. MAOIs require a 14-day washout before any SSRI or SNRI. Never guess-always follow your doctor’s exact instructions.
Can herbal supplements interact with psychiatric meds?
Yes. St. John’s Wort is a major one-it acts like an SSRI and can cause serotonin syndrome when combined with antidepressants. Kava and valerian can increase sedation when taken with antipsychotics or benzodiazepines. Even omega-3s can thin the blood, which is risky if you’re on lithium or warfarin. Always disclose every supplement you take.
Are there safer antidepressants if I’m on multiple medications?
Yes. Sertraline, citalopram, and vilazodone have lower interaction risks. Mirtazapine doesn’t affect liver enzymes much and is often used in complex cases. Your doctor can choose one based on your current meds, not just your symptoms. Avoid fluvoxamine and paroxetine if you’re on other drugs-they’re strong enzyme inhibitors.
What should I do if I miss a dose of one of my psychiatric meds?
Don’t double up. Missing one dose rarely causes immediate danger, but restarting after a gap can trigger withdrawal or interaction issues. Call your doctor or pharmacist for advice. If you’re on an MAOI or lithium, even one missed dose can throw off your balance-so always have a plan for what to do if you forget.

Shubham Semwal
November 28, 2025 AT 04:01Bro, this post is basically a pharmacology textbook with a side of panic. I’ve seen people on SSRIs pop tramadol like candy and wonder why they’re sweating like they ran a marathon in a sauna. Serotonin syndrome ain’t a myth-it’s a slow-motion car crash you didn’t see coming. And yeah, fluvoxamine? That thing’s a silent assassin. One guy I knew took it with his sleep aid and ended up in the ER with a heart rate of 140. No joke. Just… don’t be that guy.
Sam HardcastleJIV
November 29, 2025 AT 14:24One is compelled to observe, with a certain degree of intellectual disquietude, that the pharmacological landscape of modern psychiatric care has evolved into a labyrinthine architecture of unintended consequence. The confluence of monoaminergic agents, particularly in polypharmaceutical regimens, constitutes not merely a clinical challenge, but an ontological quandary regarding the boundaries of self-regulation in neurochemical equilibrium. One might posit, then, that the human psyche has become a site of pharmacological colonialism-where molecules, unmoored from ethical oversight, impose their will upon synaptic topography.
Mira Adam
December 1, 2025 AT 02:56Wow. So we’re just supposed to trust doctors who prescribe five meds and then say ‘it’s fine’? My cousin took lithium and ibuprofen for a headache and ended up in the ICU. They didn’t even ask what OTC stuff she was on. This isn’t medicine-it’s Russian roulette with a prescription pad. And don’t get me started on how often people are just handed a new drug like it’s a candy bar.
Miriam Lohrum
December 1, 2025 AT 09:57It’s fascinating how we treat the brain like a machine you can tune with pills, but then act surprised when the gears grind. We don’t ask how the body feels-we just ask if the symptoms decreased. Maybe the real problem isn’t the drugs, but the assumption that complexity can be solved with more chemistry. Sometimes, the quietest solution is less, not more.
Rebecca Price
December 2, 2025 AT 15:15Okay, real talk: if you’re on multiple psych meds, you’re not just a patient-you’re a walking drug interaction hazard zone. And honestly? That’s on us. We don’t educate people enough. I work in mental health outreach, and I’ve seen so many folks take St. John’s Wort because ‘it’s natural’ and then crash into serotonin syndrome. We need better public resources-like simple infographics, hotline numbers, maybe even pharmacy QR codes that scan your meds and flag risks. It’s not rocket science. It’s basic safety. And yes, I’m calling for systemic change. Because nobody should die because they didn’t know Benadryl could kill them when mixed with sertraline.
shawn monroe
December 4, 2025 AT 02:00GUYS. SEROTONIN SYNDROME IS NOT A DRAMA. IT’S A CODE BLUE. 🚨 I’ve seen it. I’ve held someone’s hand while they were seizing because they took tramadol + sertraline for ‘a little back pain’. The docs said ‘it’s fine’. It was NOT fine. Fluvoxamine + clozapine? That’s a nuclear option. Don’t be cute. Check your med list. Use Medscape. Use Epocrates. Use your brain. Your life is not a lab experiment. 💉🧠
marie HUREL
December 5, 2025 AT 01:14I’ve been on three meds for five years and never had an issue, but I also never start anything new without calling my pharmacist. I keep a little card in my wallet with every pill, dose, and why I take it. My mom used to say, ‘If you don’t know what’s in your body, you don’t own it.’ I think about that every time I get a new script. It’s not paranoia-it’s power.
Lauren Zableckis
December 5, 2025 AT 12:19I wish more people knew how common this is. I was on venlafaxine and took a cold med with dextromethorphan. Didn’t feel anything at first. Then I started seeing colors behind my eyes. I thought I was hallucinating. Turned out it was early serotonin syndrome. I went to urgent care and they were like, ‘Oh, that’s why you’re here.’ No one warned me. No one asked. I’m lucky I didn’t end up in ICU. Please, if you’re on antidepressants, just… Google interactions before you take anything else. Even if it’s ‘harmless’.
Asha Jijen
December 6, 2025 AT 06:00Edward Batchelder
December 6, 2025 AT 22:13I want to thank you for writing this. Honestly. I’ve been managing bipolar disorder with lithium, valproate, and quetiapine for over a decade. I’ve had three near-misses with toxicity because of NSAIDs and one doctor who didn’t check my levels for 11 months. You’re right-this isn’t about fear. It’s about precision. I carry a printed med list. I have a pharmacy alert on my phone. I ask questions. And I tell every new provider: ‘I’m on a cocktail. Don’t add to it unless you’ve checked every interaction.’ This isn’t weakness. This is survival. And if you’re on multiple meds, you’re not broken-you’re a warrior. Keep going.
reshmi mahi
December 8, 2025 AT 14:59India here. My uncle took SSRIs + St. John’s Wort + ayurvedic ‘brain tonic’ and started screaming at his mirror like it was possessed. Took him 3 days to calm down. Everyone thought he was ‘going crazy’. No one thought of drug interactions. We have zero awareness here. Even doctors don’t know. I’m just glad he’s alive. Please, if you’re from a country where ‘natural’ means ‘safe’-STOP. It’s not. 🙏
laura lauraa
December 9, 2025 AT 07:12How utterly tragic that we’ve reduced the human mind to a chemical equation-then blame the patient when the equation explodes. You’ve outlined the mechanics of a systemic failure, yet I wonder: where is the compassion? Where is the accountability? The doctors who prescribe these combinations without genetic screening, without follow-up, without even asking about herbal teas… are they healers-or corporate agents of pharmacological convenience? I am not surprised. I am merely… disgusted.
Gayle Jenkins
December 11, 2025 AT 06:29Thank you for this. I’m a nurse in a psych unit, and I’ve seen too many people come in because someone added a new med without checking their list. I make it my job to sit with every new patient and go through their meds-prescription, OTC, supplements, even tea. I’ve saved lives just by asking, ‘What else are you taking?’ I wish every doctor did this. But since they don’t, you have to be your own advocate. Keep that list. Ask the pharmacist. Speak up. You’re not being difficult-you’re being smart. And you deserve to be safe.