 Oct, 30 2025
Oct, 30 2025
Antibiotic-Steroid Risk Checker
Important Safety Information
This tool helps you understand your risk of tendon rupture when taking fluoroquinolone antibiotics with corticosteroids. Do not rely on this tool for medical diagnosis.
If you are currently taking both medications and experience tendon pain or stiffness, stop the antibiotic immediately and contact your doctor.
Your Risk Assessment
Your Risk Level
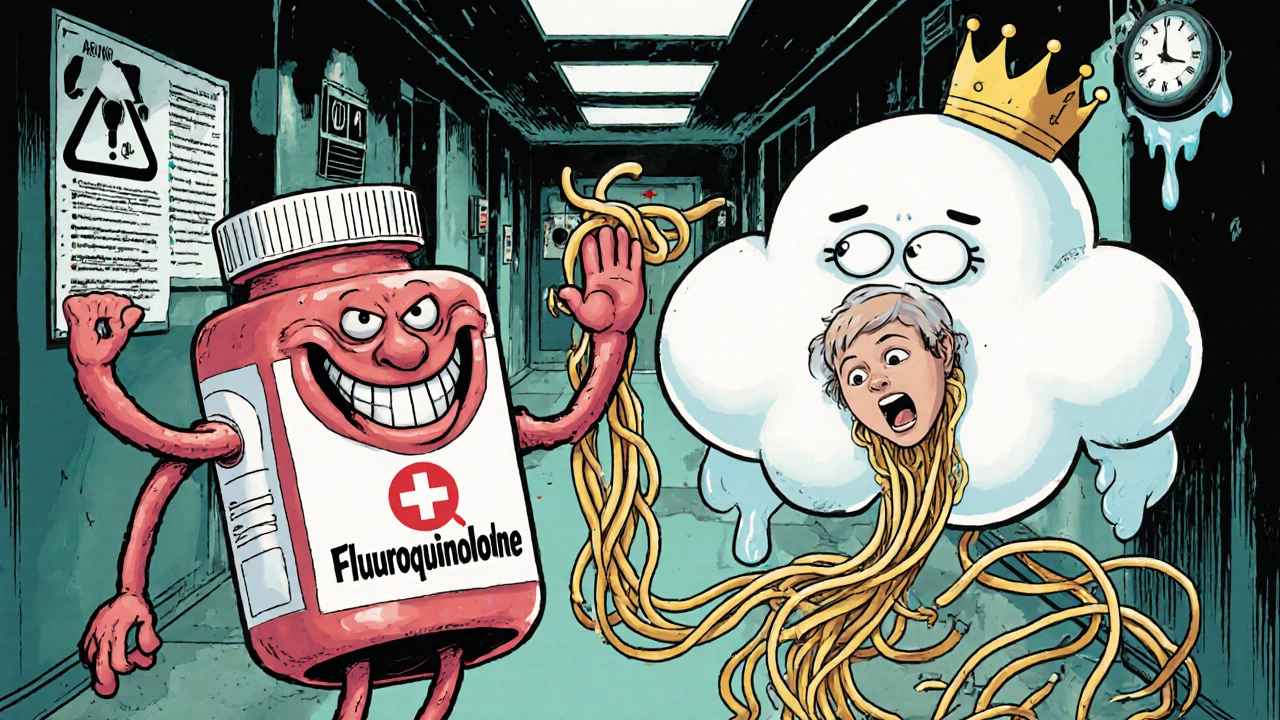
Why a Simple Antibiotic Can Break Your Tendon
You take an antibiotic because you’re sick. You get a steroid shot for your sore shoulder. Both seem harmless, routine. But when these two are combined, they can trigger something terrifying: a sudden, painful snap in your Achilles tendon-no warning, no fall, just your body giving out while you’re walking to the kitchen.
This isn’t rare. It’s not a myth. It’s a documented, deadly interaction between fluoroquinolone antibiotics and corticosteroids. And it’s happening more often than most doctors admit.
In Australia, the U.S., and across Europe, health agencies have issued black box warnings-the strongest possible alert-for this exact combination. Yet, prescriptions still happen. Patients still get hurt. Why? Because the risk feels small. But when it hits, it changes your life forever.
What Are Fluoroquinolones?
Fluoroquinolones are a class of powerful antibiotics used for stubborn infections: urinary tract infections, pneumonia, sinus infections, and sometimes even Lyme disease. Common names include ciprofloxacin, levofloxacin, and norfloxacin. They work by smashing bacterial DNA, stopping infections in their tracks.
For decades, they were considered miracle drugs-effective, oral, broad-spectrum. But since the early 2000s, a dark side emerged. Tendons started breaking. Not from trauma. Not from overuse. Just from taking the pill.
Studies show that ciprofloxacin alone accounts for nearly 70% of all reported tendon injuries linked to this drug class. In New Zealand, between 2007 and 2012, 53 cases were reported to their national drug safety system. Thirty-six of those were full ruptures. The Achilles tendon was involved in 90% of them.
How Do These Antibiotics Damage Tendons?
It’s not inflammation. It’s not an allergic reaction. It’s direct chemical damage.
Fluoroquinolones interfere with collagen-the main structural protein in tendons. They disrupt the function of tenocytes, the cells that maintain tendon strength. They also trigger enzymes that break down the tendon’s natural repair system. The result? Tendons become brittle, weak, and prone to tearing-even without stress.
What’s chilling is how fast this happens. Symptoms can start within days. The median time to tendinitis is just six days after starting the drug. And 85% of cases occur within the first month. Some patients report pain after just one dose.
Worse, the damage doesn’t stop when you finish the pills. Half of all ruptures happen after stopping the antibiotic. You think you’re safe. You’re not.
Corticosteroids: The Silent Force Multiplier
Corticosteroids-like prednisone, methylprednisolone, or even injected joint shots-are powerful anti-inflammatories. Used wisely, they help with arthritis, asthma, and autoimmune conditions. But they also weaken tendons.
They reduce collagen production. They suppress the cells that repair tissue. They make tendons more fragile. Alone, steroids increase rupture risk. Alone, fluoroquinolones do too. But together? The numbers are horrifying.
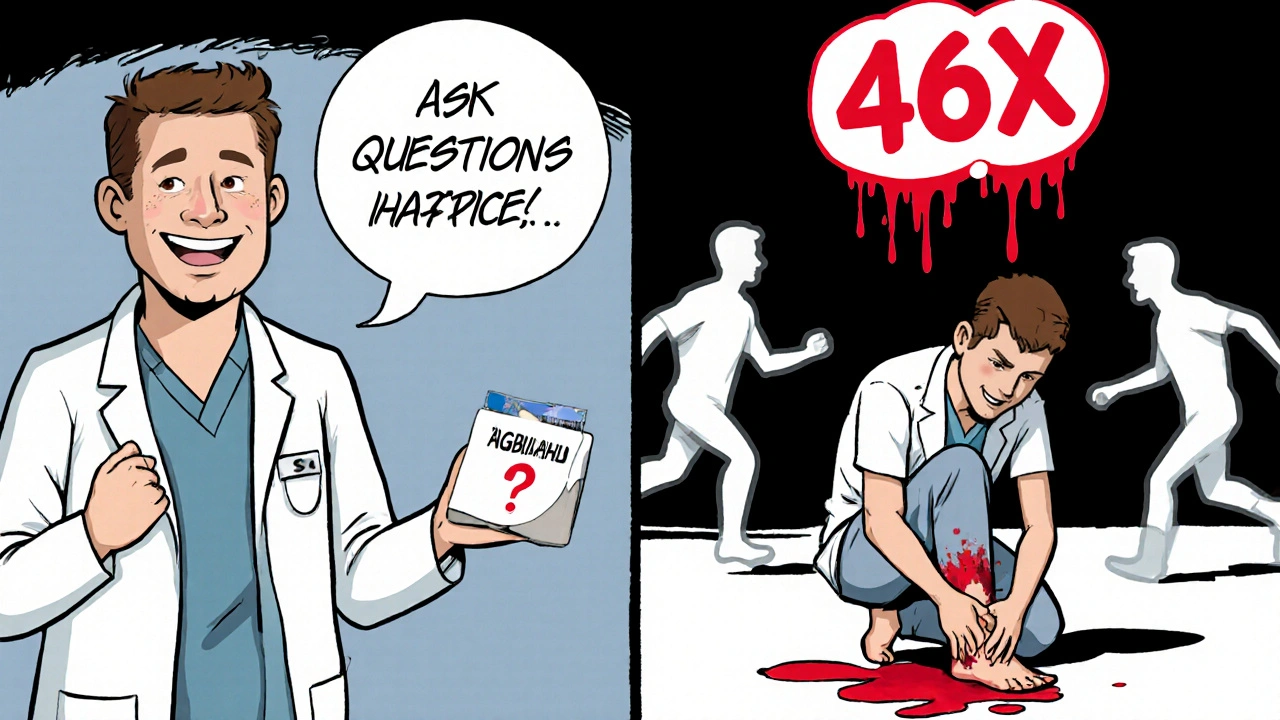
A major study published in the Journal of the American Medical Association found that when fluoroquinolones and corticosteroids are taken together, the risk of Achilles tendon rupture jumps by 46 times compared to taking neither. That’s not a typo. Forty-six times.
Compare that to other antibiotics. Penicillin? No increased risk. Amoxicillin? No link. Macrolides like azithromycin? Safe. Only fluoroquinolones carry this specific, dangerous synergy with steroids.
Who’s Most at Risk?
This isn’t about everyone. It’s about specific groups. If you fit even one of these, you’re in the danger zone:
- Age 60 or older - Risk of rupture is 2.7 times higher than in younger adults.
- On oral or injected steroids - Even a short course, like 5-7 days of prednisone, raises the danger.
- Have kidney problems - Especially if your eGFR is below 30. Fluoroquinolones build up in your system.
- Diabetic - Poor blood sugar control worsens tendon health.
- Previous tendon injury - Even if it was years ago. Your tendons never fully recover.
- Organ transplant recipient - Immunosuppressants and steroids are common here, compounding the risk.
Most patients who suffer ruptures are over 60, on steroids, and prescribed ciprofloxacin for a simple UTI. That’s the perfect storm.
What Does a Tendon Rupture Feel Like?
It doesn’t feel like a pulled muscle. It feels like a gunshot.
Patients describe a sudden, sharp pop or crack in the back of the ankle. Then, immediate weakness. You can’t push off your foot. You can’t stand on your toes. Walking becomes impossible.
Before the rupture, many have warning signs: dull ache, stiffness, swelling around the Achilles. These symptoms often appear 1-2 weeks before the tear. If you feel this while on a fluoroquinolone, stop the drug immediately and see a doctor.
Half of all ruptures are bilateral-both tendons fail. Recovery is brutal. Surgery is often needed. Rehabilitation takes 6 to 12 months. Many never return to their previous level of activity.
Why Do Doctors Still Prescribe This Combo?
Because they forget. Or because they think the risk is too low to matter.
The absolute risk of rupture from fluoroquinolones alone is low-about 0.1% to 0.4%. But when you add steroids? That risk spikes to over 4%. That’s 40 in 1,000. That’s not negligible. That’s a serious threat.
Many doctors still prescribe ciprofloxacin for uncomplicated infections-like a simple bladder infection-when safer alternatives exist. The FDA says fluoroquinolones should be reserved for infections with no other options. Yet, they’re still used as first-line for UTIs, sinusitis, bronchitis.
And steroids? Often given without thinking about the antibiotic interaction. A patient gets a knee injection for arthritis, then gets ciprofloxacin for a cough. No one connects the dots.
What Should You Do?
If you’re prescribed a fluoroquinolone, ask these questions:
- Is there a safer antibiotic? (Amoxicillin, nitrofurantoin, or trimethoprim are often fine for UTIs.)
- Am I on steroids-or will I start them soon?
- Am I over 60? Do I have diabetes or kidney issues?
- What are the signs of tendon damage? What should I do if I feel pain?
If you’re already on both drugs, stop the fluoroquinolone immediately if you feel any tendon pain, swelling, or stiffness. Don’t wait. Don’t tough it out. Call your doctor. Get an ultrasound or MRI if needed.
Never assume it’s just soreness. This isn’t muscle fatigue. This is structural failure waiting to happen.
Alternatives to Fluoroquinolones
For most common infections, safer antibiotics work just as well:
- Uncomplicated UTI: Nitrofurantoin, trimethoprim, amoxicillin-clavulanate
- Acute sinusitis: Amoxicillin, doxycycline
- Community-acquired pneumonia: Azithromycin, doxycycline
- Prostatitis: Trimethoprim, doxycycline
Fluoroquinolones still have a place-for severe infections like pyelonephritis, complicated intra-abdominal infections, or when other drugs fail. But they’re not first-line for most things.
Ask your doctor: “Is this the best choice for me, given my age and medications?” If they hesitate or dismiss you, get a second opinion.
The Bigger Picture
This isn’t just about one drug interaction. It’s about how medicine treats risk.
We’ve normalized taking pills without thinking about consequences. We assume if it’s FDA-approved, it’s safe. But safety isn’t static. New evidence emerges. Warnings are added. Prescribing habits lag behind.
Fluoroquinolones are a textbook case of a drug that was overused, then under-regulated. Even after black box warnings in 2013, prescriptions didn’t drop fast enough. Patients kept getting hurt.
The solution? Better education. Better communication. And most of all-respect for the body’s fragility. Tendons aren’t just ropes. They’re living tissue. And they can break from chemicals, not just force.
What to Do If You’ve Been Hurt
If you’ve suffered a tendon rupture after taking a fluoroquinolone-especially with steroids-you’re not alone. You’re not overreacting. You’re not crazy.
Document everything: prescription dates, symptoms, doctor visits, imaging reports. Report the reaction to your country’s drug safety agency (like TGA in Australia or FAERS in the U.S.). These reports help others avoid the same fate.
Recovery is long. But you can rebuild strength. Physical therapy is critical. Avoid returning to activity too soon. And never take fluoroquinolones again. The risk doesn’t go away after one exposure.
Can fluoroquinolones cause tendon rupture even if I’m not on steroids?
Yes. Fluoroquinolones alone increase the risk of tendon rupture by 1.3 times compared to no antibiotic use. The risk is highest in people over 60, those with kidney problems, or those with prior tendon injuries. Steroids multiply the danger, but they’re not required for the injury to occur.
How long after stopping the antibiotic can a tendon rupture happen?
Up to 50% of tendon ruptures occur after the fluoroquinolone course is finished. Symptoms can appear weeks later. There’s no safe window. If you’ve taken one of these drugs, stay alert to tendon pain for at least 3 months after stopping.
Are all fluoroquinolones equally risky?
No. Ciprofloxacin is the most commonly linked to tendon rupture, followed by norfloxacin. Levofloxacin carries risk too, but appears slightly less frequent in reports. All systemic fluoroquinolones have the same FDA black box warning. None are safe if you’re at risk.
Can I take a fluoroquinolone if I’ve had a tendon injury before?
Absolutely not. A history of tendon rupture or tendinitis is a hard contraindication. Even if it happened years ago, your tendons remain vulnerable. Doctors should avoid prescribing fluoroquinolones entirely in these cases.
What should I do if I feel pain in my Achilles while on a fluoroquinolone?
Stop the medication immediately. Do not wait for the pain to get worse. Contact your doctor or go to an urgent care clinic. Get an ultrasound to check for tendon damage. Continuing the drug can turn tendinitis into a full rupture within hours.
Final Thought: Your Tendons Can’t Talk. You Have to Speak for Them.
Antibiotics save lives. Steroids relieve pain. But medicine isn’t risk-free. Some combinations are silent killers. Fluoroquinolones and corticosteroids are one of them.
Don’t let convenience override caution. Don’t let a doctor’s habit become your tragedy. Ask questions. Push back. Demand safer options. Your next step might be a walk-or a rupture. Choose wisely.

Keerthi Kumar
November 1, 2025 AT 08:13Wow. This is the kind of post that makes you pause-really pause-between swallowing your pill and wondering if you’re being slowly sabotaged by the very system meant to heal you.
I’m from India, where antibiotics are sold over the counter like candy. My aunt took cipro for a UTI last year, got a steroid shot for her knee two weeks later, and woke up one morning unable to stand. No fall. No accident. Just… gone. The tendon didn’t just tear-it dissolved. Like chalk in water.
We don’t have black box warnings here. We have pharmacists who don’t read the leaflets. We have doctors who prescribe because it’s fast, cheap, and covered by insurance. And we have patients who believe if it’s prescribed, it’s safe.
This isn’t just a medical issue. It’s a cultural one. We’ve outsourced our health to convenience. We don’t ask questions because we’ve been trained to trust the white coat. But when your body turns against you because of a pill you took for a sniffle… that’s not negligence. That’s betrayal.
I’ve started sharing this with every older relative I know. Not as a scare tactic. As a survival guide. Your tendons aren’t replaceable. Your life isn’t a clinical trial.
Jens Petersen
November 1, 2025 AT 12:59Let me be the first to say this with the precision of a scalpel: fluoroquinolones are not antibiotics-they’re biochemical landmines disguised as pharmaceuticals.
The FDA’s black box warning? A toothless tiger. The pharmaceutical industry doesn’t care about tendon ruptures because they’re not fatal. They’re disabling. And disability doesn’t make headlines-it makes lawsuits. And lawsuits are just another line item in the quarterly report.
They’ve known since the 90s. The data was there. The case studies piled up. But why change a profitable model? Because patients are replaceable. Tendons aren’t.
And let’s not pretend this is about ‘risk-benefit.’ There is no benefit if you’re 72, diabetic, and on prednisone for polymyalgia. You’re not ‘treating’ a UTI-you’re gambling your mobility on a 1-in-25 chance of becoming a paraplegic in all but name.
Doctors who still prescribe this combo are either willfully ignorant or complicit. Either way, they should be stripped of their licenses.
Dade Hughston
November 2, 2025 AT 13:26Jim Peddle
November 4, 2025 AT 10:23There’s a reason they don’t tell you this.
It’s not incompetence. It’s control.
Fluoroquinolones are engineered to be broad-spectrum. That means they kill everything. Including your mitochondria. Your collagen. Your tendons. Your nervous system. The fact that tendon rupture is the most visible side effect is just the tip of the iceberg.
What about the chronic fatigue? The neuropathy? The anxiety that comes out of nowhere? The tinnitus that never fades? These are all documented. But they’re buried in footnotes. Because if people knew how much damage these drugs do to the *entire* body, they’d stop buying them. And the industry can’t afford that.
This isn’t a side effect. It’s a feature. A quiet, slow-motion weaponization of the human body. And the FDA? They’re just the PR arm of Big Pharma.
S Love
November 4, 2025 AT 10:41Thank you for writing this with such clarity and urgency.
I’m a physical therapist in rural Ohio. I’ve seen six patients in the last two years with fluoroquinolone-induced ruptures-all over 60, all on steroids, all prescribed cipro for a ‘simple’ UTI. One woman, 74, was a gardener. She couldn’t stand to kneel after her rupture. She cried every session because she couldn’t plant her tomatoes.
I don’t just treat tendons-I advocate. I now carry printed handouts in my bag. I ask every patient: ‘Have you taken any antibiotics in the last 30 days?’ If they say yes, I ask which one. If it’s cipro or levofloxacin, I say: ‘Stop. Now. Call your doctor. Don’t wait for pain.’
This isn’t hyperbole. It’s triage. And if your doctor pushes back? Get a second opinion. Your tendon is not a bargaining chip.
Pritesh Mehta
November 6, 2025 AT 03:02You Westerners are so dramatic. In India, we’ve been taking antibiotics like candy since the 1970s. We don’t have time to worry about tendons. We have jobs. We have families. We have to survive.
Fluoroquinolones? They’re powerful. Yes. But so is our resilience. You think your body is fragile? Look at our farmers who walk 10 kilometers to work with 50kg sacks on their backs. Their tendons don’t break because they’re not pampered. They’re forged.
And your ‘black box warnings’? That’s just another way for rich countries to scare people into compliance. We don’t need your fear. We need solutions. And solutions are not found in fear-mongering. They’re found in strength.
Maybe if you exercised more and stopped being so neurotic about pills, you wouldn’t need them in the first place.
Billy Tiger
November 6, 2025 AT 15:08Emmalee Amthor
November 7, 2025 AT 23:34Leslie Schnack
November 8, 2025 AT 08:51Could you clarify the timeline for tendon rupture after stopping the antibiotic? The post says up to 50% occur after discontinuation, but does that mean 3 months? 6 months? Is there a peak window?
Also, are there any studies comparing the risk between oral vs. IV fluoroquinolones? I’m wondering if topical application (e.g., eye drops) carries the same risk.
And-this might be a stretch-but have there been any longitudinal studies tracking tendon health in patients who took fluoroquinolones in their 30s or 40s and then later developed degenerative tendon issues in their 60s? Could this be a latent trigger for age-related decline?
Saumyata Tiwari
November 8, 2025 AT 21:57How ironic that Western medicine, which prides itself on evidence-based practice, ignores the most glaring evidence in favor of profit-driven protocols.
Fluoroquinolones were never meant for UTIs. They were designed for bio-warfare-level infections. The fact that they’re prescribed for traveler’s diarrhea is criminal. And the global south? We’re the dumping ground for expired stock and off-label use.
India doesn’t need your warnings. We need your accountability. Stop exporting your dangerous drugs to countries with weak regulation. Stop funding the marketing that convinces doctors in Lagos, Jakarta, and Mumbai that cipro is ‘the best.’
This isn’t a medical issue. It’s colonialism in pill form.
Anthony Tong
November 10, 2025 AT 21:39Statistical analysis reveals a clear pattern: the 46-fold increase cited in JAMA is derived from a small cohort with significant confounding variables-age, comorbidities, concomitant NSAID use. The absolute risk remains statistically insignificant in healthy populations under 50.
Furthermore, the FDA’s black box warning was issued in response to media hysteria, not robust epidemiological data. Prescription rates have declined 18% since 2013, yet hospitalizations for tendon rupture have remained flat-suggesting other factors dominate.
Medical overreaction is a greater threat than the drug itself. Fear drives noncompliance, which drives resistance. This is not a call to avoid fluoroquinolones. It is a call to avoid panic.
Roy Scorer
November 11, 2025 AT 11:56You know what’s worse than a ruptured tendon?
Knowing that you could’ve stopped it.
I took cipro for a sinus infection. I didn’t even have a fever. Just a stuffy nose. I was on prednisone for allergies. I didn’t think twice. I trusted the doctor. I trusted the system.
Then I woke up one morning and couldn’t stand. I thought I’d torn a muscle. I went to urgent care. They laughed. ‘You took cipro, right?’
They didn’t even look at my chart. They knew. Everyone knows. And no one told me.
Now I have a titanium anchor in my heel. I walk with a cane. I can’t run. I can’t dance. I can’t pick up my daughter.
So I’m not angry at the drug. I’m angry at the silence. The silence of the doctors. The silence of the regulators. The silence of the pharmaceutical reps who handed out free samples and never mentioned the risk.
That silence killed my mobility.
Marcia Facundo
November 12, 2025 AT 23:25S Love
November 14, 2025 AT 16:51Emmalee, your comment hits hard-and you’re not alone.
I’ve had patients tell me the same thing: ‘I didn’t know I had a right to ask.’
But here’s the truth: you do. You always have. Medicine isn’t a religion. It’s a service. And you’re the customer.
Next time you’re handed a script, say: ‘Is there a safer option?’ Say: ‘I’m on steroids.’ Say: ‘I’m 68.’ Say it like you mean it.
They’re not going to come to you with the truth. You have to pull it out of them.
Your body isn’t a passive object. It’s your home. And you’re the landlord.