 Jan, 28 2026
Jan, 28 2026
Aplastic Anemia Symptom Checker
Medication-induced aplastic anemia is rare but life-threatening. This tool helps you assess if your symptoms could indicate this condition. If you have severe symptoms or are taking high-risk medications, see a doctor immediately.
Medication Information
Symptom Assessment
When you start a new medication, you expect side effects like a headache or upset stomach-not a life-threatening collapse of your blood production. But for some people, common drugs can silently shut down bone marrow, leading to medication-induced aplastic anemia. It’s rare, but when it happens, speed saves lives. The difference between catching it early and missing it can mean the difference between recovery and death.
What Exactly Is Medication-Induced Aplastic Anemia?
Aplastic anemia isn’t just low iron or vitamin deficiency. It’s when your bone marrow stops making red blood cells, white blood cells, and platelets-all of them. This is called pancytopenia. Normally, your bone marrow churns out billions of blood cells every day. In medication-induced cases, certain drugs damage the stem cells that do this job. The damage isn’t always obvious at first. You might feel tired for weeks, think you’re just stressed, and keep going-until you start bleeding for no reason or get a fever that won’t break.
It’s not the same as chemotherapy side effects, where bone marrow suppression is expected and temporary. True aplastic anemia means your marrow stays empty even after you stop the drug. Studies show that 70% of medication-triggered cases are classified as severe. That means your neutrophil count drops below 500 per microliter, your platelets fall below 20,000, and your reticulocyte count (new red blood cells) plummets. This isn’t something you can wait out.
Which Medications Are Most Likely to Cause It?
Not every drug causes this. But some have a proven, dangerous link. The most notorious is chloramphenicol-an old antibiotic rarely used today, but still prescribed in some countries. For every 24,000 to 40,000 people who take it, one develops aplastic anemia. That’s rare, but the risk is 30 to 60 times higher than in people who don’t take it.
Other high-risk drugs include:
- Carbamazepine and phenytoin (anti-seizure meds)
- Sulfonamides and penicillin derivatives (antibiotics)
- Gold compounds (used for rheumatoid arthritis)
- NSAIDs like phenylbutazone (no longer sold in the U.S. but still used elsewhere)
- Certain antipsychotics and immunosuppressants
Here’s the tricky part: some drugs cause direct toxicity. Others trigger your immune system to attack your own bone marrow. Carbamazepine, for example, binds to proteins in your marrow and tricks your body into thinking those cells are foreign. Your immune system then destroys them. That’s why stopping the drug isn’t always enough-you may need immune-suppressing treatment too.
Early Signs You Can’t Ignore
Most people don’t wake up one day with aplastic anemia. It creeps in. The first warning signs are often mistaken for the flu, stress, or aging.
Here’s what to watch for-especially if you’ve started a new medication in the past 6 weeks:
- Persistent fatigue that doesn’t improve with rest. Not just tired-you feel drained even after sleeping.
- Unexplained bruising, especially multiple bruises appearing at once without injury.
- Bleeding gums or nosebleeds that won’t stop easily.
- Recurrent low-grade fevers (99-101°F) that come and go for days.
- Shortness of breath during normal activities like walking to the mailbox.
- Unintentional weight loss (5-10 pounds over 2-3 weeks).
- Prolonged infections-a cold that won’t clear, or a minor cut that gets infected easily.
Here’s what patients often say: “I thought I was just run down.” That’s the most common response in surveys. In fact, 68% of patients with medication-induced aplastic anemia report symptoms for 4 to 6 weeks before diagnosis. And in 72% of cases, their doctor first thought it was a virus.
Why Timing Is Everything
Dr. Neal Young from the NIH says this clearly: “Early recognition is the single most important factor determining survival.” If you catch it within two weeks of symptoms starting, your survival rate is under 10%. If you wait eight weeks? It jumps to 45%.
Why? Because your body is running out of defenses. Platelets keep you from bleeding. Neutrophils fight infections. When those numbers crash, you’re one cough away from sepsis. And once you get a serious infection with neutrophils below 500, you need hospitalization-fast.
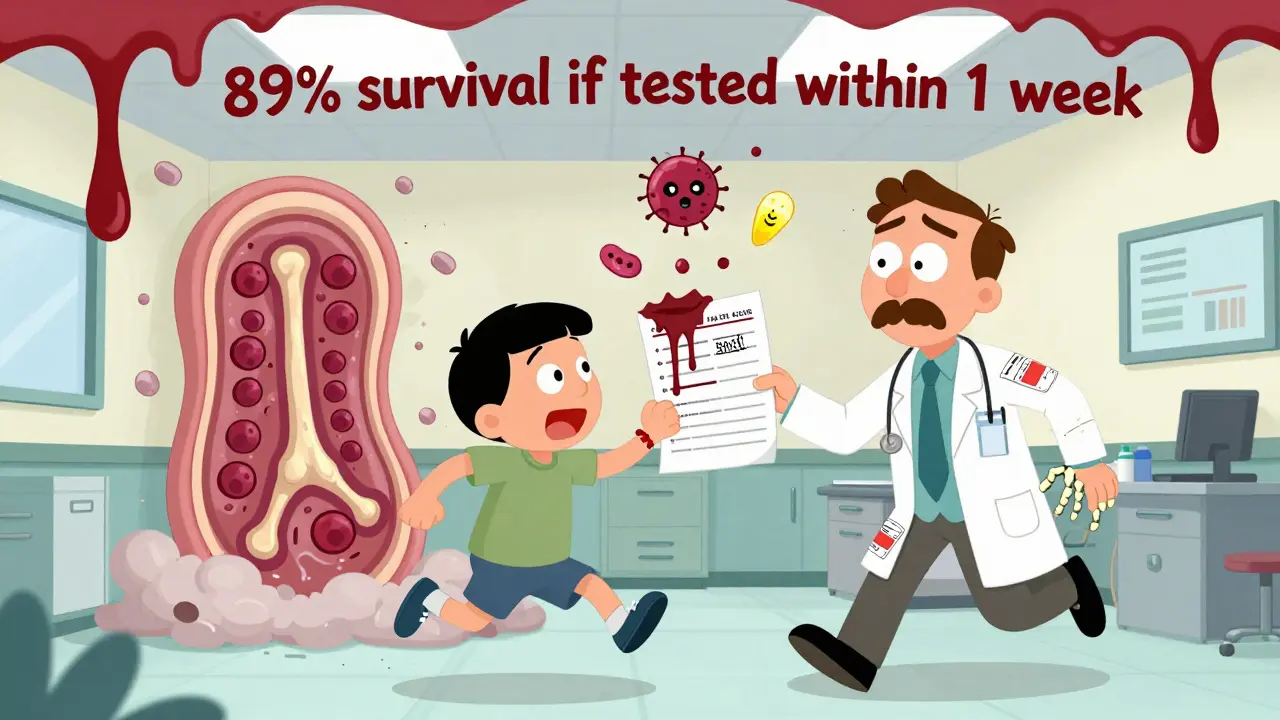
One study showed that patients who got a blood test within one week of noticing symptoms had an 89% survival rate. Those who waited three weeks? Only 62%. That’s not a small gap. That’s life or death.
What To Do Immediately If You Suspect It
If you’re on one of these high-risk medications and you’re experiencing two or more of the early signs above, here’s what you do-right now:
- Stop taking the medication. Do not wait for a doctor’s appointment. Call your prescriber or pharmacist immediately. Discontinuing the drug is the first and most critical step. In mild cases, blood counts can bounce back in four weeks.
- Get a CBC (complete blood count) within 24 hours. Don’t wait for a routine check-up. Go to an urgent care or ER if your clinic can’t do it same-day. Look for hemoglobin under 10 g/dL, platelets under 150,000/μL, or neutrophils under 1,500/μL. These are the red flags.
- If platelets are below 50,000/μL, see a hematologist immediately. If they’re below 10,000/μL or you’re bleeding, you need transfusions. Don’t delay.
- If you have a fever above 100.4°F (38°C), go to the ER. Now. This is a medical emergency. You could be developing a life-threatening infection with no immune defense.
- Bring your full medication list. Include supplements, herbal products, and over-the-counter drugs. Many cases are missed because doctors don’t know you’re taking something like an NSAID or an antibiotic you got abroad.
And here’s something patients rarely think to do: keep a written record of every medication you’ve taken in the last 12 months. One study found that having this list reduced diagnostic delays by over six days. That’s six days you might have saved your life.

What Happens After Diagnosis?
If your CBC shows pancytopenia, you’ll need a bone marrow biopsy. That’s the only way to confirm aplastic anemia. The marrow should be less than 25% full of cells. Normal marrow is 60-80% full. If it’s empty, you have aplastic anemia.
Treatment depends on severity:
- Mild cases: Just stopping the drug and monitoring. Blood counts often recover on their own.
- Severe cases: Immunosuppressive therapy-usually horse anti-thymocyte globulin (ATG) plus cyclosporine. This stops your immune system from attacking your marrow. Response rates are around 78%.
- Very severe cases: Bone marrow transplant, especially if you’re under 40 and have a matched donor. This is the only cure.
And here’s a hard truth: if you restart the drug that caused it-even after you’ve recovered-there’s a 90% chance you’ll get it again, and worse. Never take it again. Not even once.
How to Protect Yourself Before Starting High-Risk Drugs
If you’re about to start carbamazepine, chloramphenicol, or any other drug linked to bone marrow failure, ask your doctor:
- “Is there a safer alternative?”
- “Can we do a baseline CBC before I start?”
- “Will you schedule weekly blood tests for the first month?”
Most clinics don’t do this automatically. But according to the American Society of Hematology, patients who get pre-treatment education are 3.5 times more likely to recognize symptoms early. Ask for a printed handout. Save it. Know what to look for.
Some hospitals now use electronic alerts that flag high-risk prescriptions and auto-schedule follow-up blood work. But not all do. If yours doesn’t, you have to be your own advocate.
What’s Changing in 2026?
There’s new hope. In 2023, the AAMDS Foundation launched a mobile app that lets patients log symptoms and blood counts. Early users saw a 40% drop in diagnostic delays. The NIH is testing a genetic test that can predict who’s at highest risk before they even take the drug. And AI systems are being trained to spot early patterns in blood counts-before doctors even notice.
Regulatory agencies are also acting. The European Medicines Agency now requires stronger warnings on carbamazepine labels. The FDA is pushing drugmakers to monitor bone marrow toxicity during clinical trials. But these changes take time. Right now, the best protection is still you.
Medication-induced aplastic anemia isn’t common. But when it happens, it’s fast, silent, and deadly. The good news? You can stop it-if you know the signs, act fast, and don’t wait for someone else to tell you it’s serious. Your body is giving you signals. Listen.
Can you get aplastic anemia from over-the-counter drugs?
Yes. While most cases are linked to prescription drugs like carbamazepine or chloramphenicol, some over-the-counter NSAIDs-especially phenylbutazone-have been tied to aplastic anemia. Even common painkillers like ibuprofen or naproxen carry a very low risk in rare cases, particularly with long-term, high-dose use. The key isn’t whether a drug is prescription or not-it’s whether it’s known to affect bone marrow.
How long after taking a drug does aplastic anemia start?
It usually appears between 2 and 12 weeks after starting the medication. Some cases show up as early as 10 days, especially with drugs like chloramphenicol. Others take months. The timing varies by drug and how your body reacts. That’s why monitoring blood counts weekly for the first month is critical if you’re on a high-risk drug.
Is aplastic anemia from medication reversible?
In mild cases, yes-if you stop the drug early. Many patients see their blood counts return to normal within 4 to 8 weeks. But in severe cases, the damage is often permanent without treatment like immunosuppressive therapy or a bone marrow transplant. The key is catching it before the marrow is too damaged to recover.
Can you get aplastic anemia from antibiotics like amoxicillin?
Amoxicillin is not a common cause, but penicillin derivatives and sulfonamides (like Bactrim) are. While amoxicillin carries minimal risk, any antibiotic can trigger an immune reaction in rare cases. The risk is higher with older drugs like chloramphenicol or sulfa-based antibiotics. Always report unusual fatigue or bruising after starting any antibiotic.
Should I get my blood tested if I’m on carbamazepine?
Absolutely. Carbamazepine increases your risk of aplastic anemia by about 15 times. Guidelines recommend a baseline CBC before starting, then weekly blood tests for the first 4 weeks. After that, monthly checks for at least 6 months. Many doctors skip this. Don’t assume they’ll order it-ask for it.
Can children get medication-induced aplastic anemia?
Yes. Children are not immune. In fact, 65% of pediatric cases are delayed because symptoms are mistaken for normal childhood illnesses-like a virus or growing pains. If your child is on an anti-seizure drug like carbamazepine or phenytoin and develops unexplained tiredness, bruising, or frequent infections, get a CBC right away.
