 Nov, 29 2025
Nov, 29 2025
Over 100 types of arthritis exist, but if you’re experiencing joint pain, you’re most likely dealing with either osteoarthritis or rheumatoid arthritis. These two aren’t just different versions of the same thing-they’re completely different diseases with different causes, symptoms, and treatments. Getting them mixed up can lead to the wrong care, unnecessary pain, and even permanent damage. Here’s what you actually need to know to tell them apart-and what to do next.
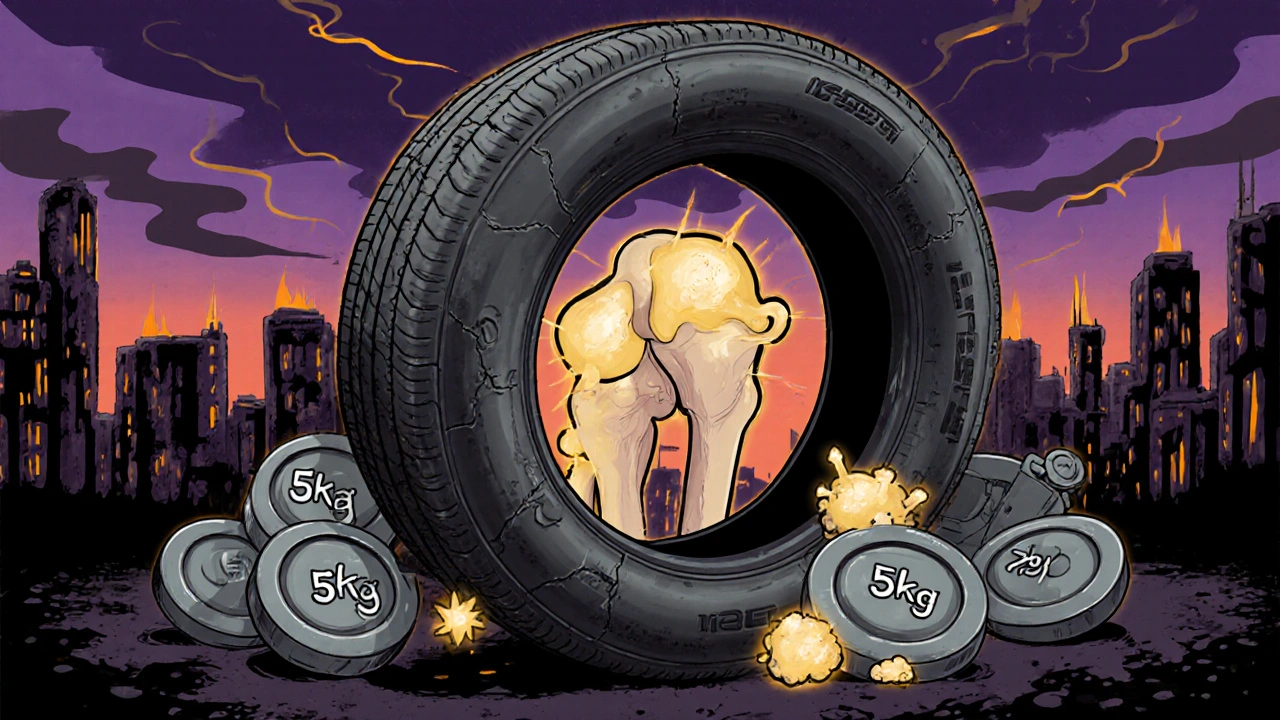
Osteoarthritis: The Wear-and-Tear Joint Breakdown
Osteoarthritis (OA) is what happens when the cushioning cartilage between your bones wears down over time. It’s not just "getting old"-it’s mechanical stress, injury, or excess weight slowly breaking down the joint’s natural shock absorber. Think of it like the tread on a tire. The more you drive, the more it wears. Same with your knees, hips, or fingers.
It usually shows up after 50, but it’s not rare in younger people who’ve had joint injuries or carry extra weight. A 5kg weight loss can cut knee OA pain by half. That’s not a guess-it’s backed by clinical data from ArthritisCARE.
OA pain gets worse when you move the joint and improves with rest. Morning stiffness? It’s usually under 30 minutes. You’ll notice it in your knees, hips, lower back, and the joints closest to your fingertips (DIP joints). You might even feel bony lumps forming around your knuckles-those are bone spurs, not swelling.
Diagnosis is straightforward: an X-ray shows narrowing joint space and bone spurs. Blood tests? Usually normal. That’s because OA isn’t an immune disease. It’s local. It stays in the joint.
Treatment? Focus on protecting the joint. Physical therapy, weight control, NSAIDs for pain, and sometimes cortisone shots. If it gets bad enough, joint replacement is common-90% of all hip and knee replacements in the U.S. are for OA.
Rheumatoid Arthritis: Your Immune System Turns on You
Rheumatoid arthritis (RA) isn’t about wear and tear. It’s about your body attacking itself. Your immune system, which should fight germs, mistakes your joint lining (synovium) for an invader and starts bombing it. That causes inflammation-swelling, heat, pain-and eventually destroys cartilage and bone.
RA can hit at any age-even in teens and young adults. Juvenile idiopathic arthritis is just RA that starts before 16. It doesn’t care if you’re active or sedentary, overweight or thin. Genetics and smoking are big risk factors. Smokers are two to three times more likely to develop RA.
Here’s the telltale sign: symmetrical joint pain. If your left wrist hurts, your right one will too. It targets the knuckles (MCP joints), wrists, and sometimes ankles. You won’t usually see DIP joint involvement-that’s more OA’s territory.
Morning stiffness? Lasts over an hour, sometimes all day. You’ll feel exhausted, maybe have a low fever, lose weight, or get dry eyes. RA doesn’t just hurt joints-it affects your lungs, heart, and even your skin (rheumatoid nodules under the skin are a red flag).
Diagnosis needs blood tests. Rheumatoid factor (RF) and anti-CCP antibodies are the big ones. Ultrasound and MRI are now used to catch early damage before X-rays show anything. The American College of Rheumatology recommends this aggressive approach because RA can destroy joints in months if untreated.
Treatment? It’s urgent. You need disease-modifying drugs (DMARDs) like methotrexate, and sometimes biologics that target specific parts of your immune system. These aren’t painkillers-they stop the attack. Biologics cost $20,000 to $50,000 a year, but they can put RA into remission in 30-50% of patients. Delay treatment, and you risk permanent deformity.
Other Common Arthritis Types You Should Know
OA and RA make up most cases, but other types are just as important to recognize.
Gout hits suddenly-often at night-with intense pain, redness, and swelling in one joint, usually the big toe. It’s caused by uric acid crystals building up. Diet matters: red meat, alcohol, and sugary drinks raise your risk. Treatment involves anti-inflammatories and long-term meds to lower uric acid.
Psoriatic arthritis shows up in people with psoriasis (that scaly skin condition). It can cause swollen fingers that look like sausages, and pain where tendons attach to bone (enthesitis). It often affects the spine too. Treatments overlap with RA-DMARDs and biologics work well.
Ankylosing spondylitis is a type of inflammatory arthritis that targets the spine and pelvis. It causes back pain and stiffness, especially in the morning. It’s more common in men and often starts in early adulthood. HLA-B27 gene testing helps confirm it.
And then there’s juvenile idiopathic arthritis-the term for arthritis in kids under 16. It can affect growth, cause eye inflammation, and needs pediatric rheumatology care.
Why Getting the Diagnosis Right Matters
Taking an NSAID for RA might ease pain for a while, but it won’t stop the joint destruction. Taking methotrexate for OA? That’s dangerous-it suppresses your immune system for no reason.
Doctors miss the difference sometimes. Hand pain? Could be OA’s bony lumps-or RA’s swollen MCP joints. One study found that nearly 1 in 5 RA cases were initially misdiagnosed as OA. That delay can mean the difference between mild symptoms and a wheelchair.
Early RA treatment within the first 3-6 months gives you the best shot at remission. OA management is about slowing decline-keeping you moving, reducing pressure on joints, avoiding surgery longer.
There’s also a big cost difference. OA treatments are mostly low-cost: physical therapy, painkillers, maybe a knee brace. RA? Biologics cost tens of thousands a year. Insurance coverage, access to rheumatologists, and timely diagnosis make a huge difference in outcomes.

What You Can Do Today
If you’re wondering whether your joint pain is OA or RA, start with these steps:
- Track your symptoms: When does the pain happen? How long is morning stiffness? Is it on both sides?
- Check for red flags: Unexplained fatigue, fever, weight loss, or skin rashes? That leans toward RA.
- See your doctor and ask for blood tests (RF, anti-CCP) and an X-ray. Don’t accept a diagnosis based on pain alone.
- If RA is suspected, push for a referral to a rheumatologist. Time is critical.
- If it’s OA, focus on weight control, strengthening muscles around the joint, and avoiding high-impact activities.
And if you’re over 50 and overweight? Losing even 5kg can dramatically reduce your knee pain. It’s not magic-it’s physics. Less weight = less pressure = less wear.
There’s no cure for either condition, but both can be managed. OA doesn’t have to mean giving up walking. RA doesn’t have to mean lifelong pain. With the right diagnosis, you can live well.
Can you have both osteoarthritis and rheumatoid arthritis at the same time?
Yes. It’s not common, but it happens. Someone with RA can develop OA in a joint that’s already damaged from years of inflammation. Or someone with OA from an old injury might later develop RA due to genetic or environmental triggers. The key is tracking symptoms-new swelling, fatigue, or symmetrical pain in someone with known OA should raise suspicion for RA.
Does weather affect arthritis pain?
Many people report worse pain in cold, damp weather. Studies show a small but real link between barometric pressure changes and joint discomfort, especially in OA. It doesn’t make the disease worse-it just makes the pain feel stronger. Staying warm and moving regularly helps more than any supplement.
Is arthritis hereditary?
OA has a weak genetic link-your risk goes up if your parents had it, especially in the hands. RA is more strongly tied to genes, particularly HLA-DRB1. But genes alone don’t cause it. Smoking, infection, or stress can trigger RA in people with the right genetic makeup. You don’t inherit arthritis-you inherit a higher risk.
Can diet help with arthritis?
For OA, losing weight is the #1 dietary fix. For RA, anti-inflammatory diets (rich in fish, olive oil, vegetables, nuts) may reduce flare-ups slightly, but they won’t replace medication. Avoiding sugar and processed foods helps everyone. Gout? Cut back on red meat, shellfish, and alcohol. No diet cures arthritis-but good nutrition supports better outcomes.
Are joint supplements like glucosamine worth taking?
For OA, studies show mixed results. Some people feel better, others don’t. It’s safe for most, so if you want to try it, go ahead-but don’t expect miracles. It doesn’t work for RA. The real power is in movement, weight control, and proven meds-not pills from the health store.
Can you stop taking RA meds once you feel better?
Never stop without talking to your rheumatologist. Even if you’re in remission, stopping DMARDs or biologics can cause a flare-and once joints are damaged, they don’t heal. Some people can reduce doses over time, but most need to stay on treatment long-term to keep the disease under control.
Final Thoughts: Know Your Body, Ask the Right Questions
Arthritis isn’t one disease. It’s a group of conditions with different causes, different risks, and different treatments. Mistaking RA for OA delays life-changing care. Confusing OA with gout leads to unnecessary suffering.
If you’ve been told you have arthritis but don’t know which kind, ask for the details. What tests were done? What’s the plan? What’s the goal? Don’t settle for a label without understanding what it means.
Whether it’s your knees, your hands, or your back-knowing the difference between wear-and-tear and immune attack is the first step to taking back control.

Tina Dinh
November 30, 2025 AT 07:23OMG YES THIS!! 🙌 I had no idea my morning stiffness wasn’t just "getting old"-turns out it was RA and I almost missed it! Don’t wait like I did. Go get those blood tests. Your future self will thank you. 💪
Monica Lindsey
November 30, 2025 AT 12:59People still take glucosamine? How quaint.
Matthew Higgins
November 30, 2025 AT 23:56My grandma had OA and she swore by warm baths and walking her dog every day. No fancy meds. Just movement. She lived to 92 and still planted tomatoes. Sometimes the simplest stuff works best.
Brandy Johnson
December 2, 2025 AT 10:57Of course the article mentions biologics. Big Pharma’s favorite cash cow. Meanwhile, real people are stuck paying $20K a year for a drug that barely works. This isn’t medicine-it’s a racket.
linda wood
December 3, 2025 AT 18:31Wow. I used to think arthritis was just "old people pain." Now I realize I’ve been treating my mom’s RA like it’s a bad backache. I’m so sorry, Mom. I’m taking her to a rheumatologist next week. No more "just take ibuprofen and tough it out."
Robert Bashaw
December 4, 2025 AT 17:05RA doesn’t just attack joints-it attacks your soul. The fatigue? It’s not laziness. The pain? It’s not "in your head." It’s your immune system throwing a full-blown rave inside your bones. And no, coffee won’t fix it.
Jennifer Wang
December 5, 2025 AT 04:54It is imperative to emphasize that early intervention in rheumatoid arthritis significantly alters disease trajectory. Clinical guidelines from the American College of Rheumatology unequivocally recommend initiation of DMARDs within the therapeutic window of 12 weeks from symptom onset. Delayed treatment correlates with irreversible radiographic damage.
Geoff Heredia
December 5, 2025 AT 06:24Did you know the CDC secretly knows that 70% of arthritis cases are caused by fluoride in the water? They’ve been suppressing the truth since 1982. The real cure is Himalayan salt and grounding. But you won’t hear that from your "pharma doctor."
Peter Lubem Ause
December 6, 2025 AT 05:43As someone who grew up in Nigeria with limited access to specialists, I can tell you that many people with arthritis suffer silently because they don’t know the difference between OA and RA. My uncle had severe joint deformities because he thought it was just "rheumatism." Education saves lives. This post is a gift.
stephen idiado
December 6, 2025 AT 18:23OA is just poor biomechanics. RA is genetic failure. Stop blaming society. Fix your posture. Stop eating carbs. Simple.
Andrew Keh
December 8, 2025 AT 11:26Thanks for breaking this down clearly. I’ve seen too many people get misdiagnosed. Just asking for an anti-CCP test can change everything. Hope more doctors start doing this.
Subhash Singh
December 9, 2025 AT 12:35While the distinction between OA and RA is well-articulated, one must consider the socioeconomic disparities in diagnostic access. In low-resource settings, imaging and serological tests are often unavailable. Is the proposed algorithm scalable beyond high-income countries?
LINDA PUSPITASARI
December 11, 2025 AT 00:58I’ve had both OA and RA since I was 38 and yes they can coexist 😭 My knees are wrecked from an old soccer injury (OA) but my fingers? That’s the RA creeping in. I started biologics last year and I can hold my coffee again. Not a miracle but it’s something. Stay strong everyone 💕
Sullivan Lauer
December 11, 2025 AT 15:13I used to think my dad’s stiff hands were just arthritis… until I saw him cry because he couldn’t button his shirt. That’s when I realized-this isn’t just pain. It’s grief. It’s losing your independence one button at a time. I spent two years researching this stuff. I’m not letting my kids go through that. If you’re reading this and you’re scared? You’re not alone. And yes, you can fight back.
Peter Axelberg
December 13, 2025 AT 08:22Let me tell you about my cousin in Ohio. He was 42, worked construction, started getting pain in his knuckles. Doctor said "it’s OA, you’re just worn out." Six months later he couldn’t grip a wrench. Blood test showed anti-CCP positive. RA. He’s on Humira now. Lost his job. Lost his truck. But he’s alive. And he’s not giving up. If you think your pain is just aging, you’re wrong. Get tested. Don’t wait until you’re holding your coffee with both hands like a toddler.