 Dec, 10 2025
Dec, 10 2025
Clozapine Dose Adjustment Calculator
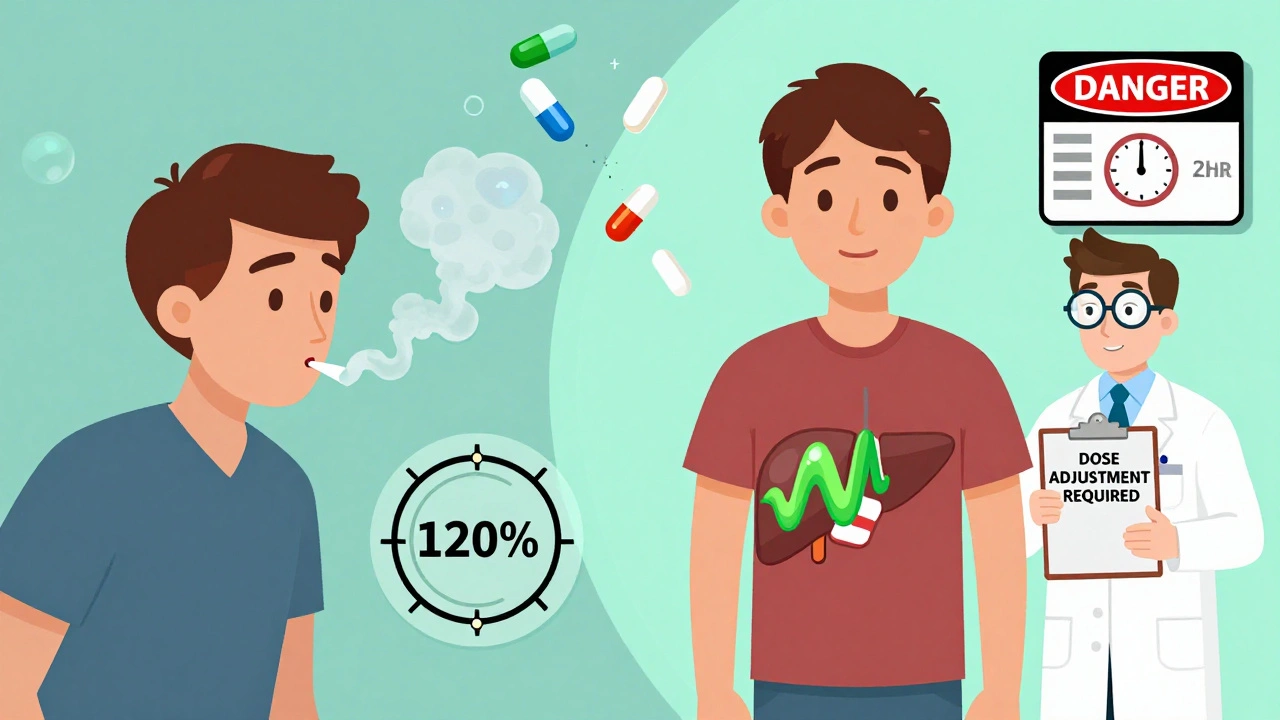
How Smoking Affects Your Medication
Clozapine is metabolized primarily by the CYP1A2 enzyme in your liver. Tobacco smoke increases this enzyme by 30-50%, which means your body breaks down clozapine faster. If you start smoking, you'll likely need a higher dose. If you quit, your dose needs to be reduced to avoid toxicity.
When you’re taking clozapine for treatment-resistant schizophrenia, your life already comes with a lot of variables. Sleep. Diet. Stress. Therapy. But one thing many patients don’t realize is that smoking can dramatically change how well your medication works-sometimes in dangerous ways.
It’s not just about cravings or lung health. Tobacco smoke directly interferes with how your body breaks down clozapine. If you smoke, your clozapine levels can drop by 30% to 50%. That means your symptoms might come back even if you’re taking the same dose. And if you quit smoking suddenly? Your levels can spike, leading to serious side effects like seizures, extreme drowsiness, or even heart problems.
Why Smoking Changes Clozapine Levels
Clozapine is mostly broken down by an enzyme in your liver called CYP1A2. This enzyme is like a factory worker-its job is to process the drug so your body can get rid of it. But tobacco smoke doesn’t just pass through your lungs. It sends chemical signals that tell your liver to make more CYP1A2. More enzyme means faster breakdown. Faster breakdown means less clozapine in your blood.
The active ingredients in cigarette smoke-things like polycyclic aromatic hydrocarbons-bind to a receptor in your liver called AhR. That switch flips on the CYP1A2 gene, turning up production. Within 48 to 72 hours of starting to smoke, your body is already clearing clozapine faster. This isn’t a myth. It’s been proven in dozens of clinical studies, including one published in Nature in 2020 that showed CYP1A2 handles 60-70% of clozapine metabolism, far more than any other enzyme.
Compare that to other antipsychotics. Olanzapine is also affected, but less so. Risperidone? Barely. Clozapine is uniquely vulnerable because it relies so heavily on just one enzyme. And it has a narrow therapeutic range: 350 to 500 ng/mL. Go below that, and symptoms return. Go above, and toxicity kicks in.
How Much Does Smoking Really Lower Clozapine?
Studies vary, but the numbers are consistent: smokers need higher doses. On average, a person who smokes 10 or more cigarettes a day will need 40-60% more clozapine than a non-smoker to reach the same blood level.
Real-world examples show this clearly. One patient on Reddit reported his clozapine level dropped from 400 ng/mL to 150 ng/mL after he started smoking. His dose had to jump from 300 mg to 500 mg just to feel stable again. Another case in SAGE Open Medical Case Reports described a 32-year-old man on 450 mg daily who still had subtherapeutic levels-until his dose was increased to 650 mg.
But here’s the flip side: when people quit smoking, their CYP1A2 activity drops back down over 1-2 weeks. If their dose stays the same, clozapine builds up. A 45-year-old woman in a 2022 case study was taking 400 mg daily. After quitting smoking, her level soared to 850 ng/mL. She became severely sedated, her heart raced, and she nearly needed ICU care. Her dose had to be cut in half-to 250 mg.
Genetics Make It Even More Complicated
Not everyone responds the same way. Some people have a genetic variant called CYP1A2 *1F/*1F. They start with normal enzyme levels, but when they smoke, their CYP1A2 shoots up even more than average. That means they might need bigger dose increases-or face higher risk of toxicity if they quit.
Other genes matter too. CYP3A4 helps break down clozapine-N-oxide, a metabolite that’s less active than clozapine. People with low CYP3A4 activity end up with higher clozapine levels even without smoking. So your genetics, your smoking habits, and your current dose all interact in unpredictable ways.
This is why blanket advice like “just take more” doesn’t work. You need personalized monitoring.
What Psychiatrists Do in Practice
Most experienced psychiatrists check smoking status at every visit. A 2023 survey of clinicians on Doximity found that 68% routinely ask about tobacco use when managing clozapine, and 82% adjust doses based on changes.
Here’s what a typical protocol looks like:
- Get a baseline clozapine blood level before any dose change.
- If a patient starts smoking, increase the dose by 40-60%. Recheck levels after 7 days.
- If a patient quits smoking, reduce the dose by 30-50%. Monitor closely for 14 days.
- Never change the dose without checking levels first.
Some hospitals now use electronic health record alerts. A 2023 study in JAMA Internal Medicine showed these automated warnings cut adverse events by 37%. That’s huge-especially when you consider that unmanaged interactions lead to 22% higher hospitalization rates, costing an average of $14,500 per avoidable admission.
What About Vaping or Nicotine Patches?
Many patients think switching to vaping or nicotine gum avoids the problem. It doesn’t.
A 2024 study from the University of Toronto found that e-cigarettes induce CYP1A2 just like traditional cigarettes-just slightly less. About 15-20% less. So if you’re vaping, you still need to adjust your clozapine dose.
Nicotine patches? They don’t trigger CYP1A2 induction. That’s good news. If you’re using patches to quit smoking, your clozapine levels won’t suddenly drop. But if you stop the patches and go back to smoking? That’s when the enzyme spikes again.
So the rule is simple: if you’re using any form of inhaled nicotine-cigarettes, cigars, pipes, vapes-you’re affecting your clozapine levels.
What If You Can’t Quit Smoking?
It’s not easy. People with schizophrenia smoke at rates 3-4 times higher than the general population. About 60-70% of clozapine users smoke. That’s not because they’re weak-it’s because nicotine temporarily eases some of the cognitive and negative symptoms of schizophrenia.
But quitting doesn’t mean you have to lose your stability. The key is planning. Work with your doctor. Don’t try to quit cold turkey while your clozapine dose is high. Instead:
- Start by lowering your dose gradually as you cut back on smoking.
- Use nicotine replacement (patches or gum) to avoid sudden drops in CYP1A2 activity.
- Check your clozapine levels before, during, and after quitting.
- Be ready to reduce your dose by 30-50% once you’ve stopped smoking for 1-2 weeks.
One patient on PatientsLikeMe wrote: “I’ve tried to quit three times. Each time, I ended up hospitalized because my clozapine levels went toxic before my doctor noticed.” That’s preventable.

Are There Alternatives to Clozapine?
Yes-but they’re not better. Clozapine is the most effective antipsychotic for treatment-resistant schizophrenia. Nothing else works as well for the 30% of patients who don’t respond to other drugs.
Quetiapine and aripiprazole are metabolized by different enzymes (CYP3A4 and CYP2D6), so they’re not affected by smoking. But they’re less effective for severe cases. Switching might mean losing symptom control.
That’s why most experts keep patients on clozapine-even if they smoke-and manage the interaction instead of switching drugs.
What’s New in 2025?
There’s promising research. A 2024 clinical trial (NCT05678901) tested a new slow-release clozapine formulation. Early results showed 40% less fluctuation in blood levels among smokers. That could mean fewer dose adjustments and fewer hospitalizations.
Pharmacogenetic testing is also becoming more common. In 2018, only 15% of U.S. academic centers tested for CYP1A2 variants. By 2023, that jumped to 47%. It’s not routine yet-but if you’ve had trouble with clozapine dosing, ask your doctor if genetic testing is an option.
The FDA now treats this interaction as a model case for how environment, genes, and drugs interact. That means more attention, better guidelines, and smarter tools are coming.
Bottom Line: Know Your Numbers
If you’re on clozapine and you smoke-or you’re thinking about quitting-this isn’t something you can wing. You need data. You need blood tests. You need a doctor who understands CYP1A2.
Don’t assume your dose is right just because you’ve been on it for years. If you started smoking last month, your levels are probably too low. If you quit last week, they might be too high.
The good news? This interaction is well understood. It’s predictable. It’s manageable. But only if you treat it like the medical issue it is-not a lifestyle footnote.
Check your levels. Talk to your doctor. Don’t change your smoking habits without a plan. Your stability-and your safety-depend on it.

Aileen Ferris
December 11, 2025 AT 21:20Sarah Clifford
December 13, 2025 AT 15:17Ben Greening
December 13, 2025 AT 17:53Ariel Nichole
December 14, 2025 AT 17:21john damon
December 15, 2025 AT 15:56matthew dendle
December 17, 2025 AT 03:31Monica Evan
December 17, 2025 AT 12:24Taylor Dressler
December 18, 2025 AT 10:45Aidan Stacey
December 18, 2025 AT 20:50Jean Claude de La Ronde
December 20, 2025 AT 13:28