 Dec, 4 2025
Dec, 4 2025
Most parents notice their baby’s dry, red, itchy skin and think it’s just a rash. But for many, that rash is the first sign of something bigger - a chain reaction called the atopic march. It’s not a guarantee, but it’s a pattern: eczema shows up in infancy, then food allergies, then asthma, then hay fever. For decades, doctors treated these as separate problems. Now we know they’re connected - and the key might be in the skin.
What Exactly Is the Atopic March?
The atopic march isn’t a straight line. It’s not a rule. It’s a trend - one that happens in only about 3.1% of children with eczema, according to recent studies. That means most kids with dry, flaky skin won’t go on to develop asthma or peanut allergies. But for the ones who do, the pattern often starts the same way: cracked skin in the first few months of life. That cracked skin isn’t just uncomfortable. It’s a doorway. Allergens like peanut proteins, egg, or dust mites slip through those tiny breaks in the skin barrier. The immune system, still learning how to respond, sees these as invaders. It starts making IgE antibodies. That’s the trigger for sensitization - the body remembers the allergen as dangerous. Later, when the child eats peanut or breathes in dust, the immune system overreacts. That’s when symptoms show up: hives, wheezing, runny nose. The big shift in understanding? It’s not that eczema causes asthma. It’s that both come from the same root: a weak skin barrier and an overactive immune system. Genetics play a huge role. Mutations in the filaggrin gene - found in up to 50% of kids with severe eczema - break down the skin’s natural protective layer. Without enough filaggrin, moisture escapes, irritants get in, and the immune system goes on high alert.Why Skin Barrier Care Isn’t Just About Moisturizing
You’ve heard it before: “Use lotion.” But skin barrier care isn’t about slathering on any cream. It’s about repairing the structure that keeps allergens out. Think of your baby’s skin like a brick wall. Filaggrin is the mortar. When it’s missing, gaps open up. Emollients - thick, fragrance-free creams or ointments - act like temporary mortar. They seal the cracks, lock in moisture, and reduce inflammation. That’s why daily application from birth, especially in high-risk babies (those with a family history of eczema, asthma, or food allergies), can cut eczema risk by 20-30%, as shown in the PreventADALL trial. It’s not magic. It’s physics. A well-hydrated, intact skin barrier doesn’t let allergens sneak in. That means fewer immune signals, less sensitization, and a lower chance of triggering the next step in the march. But here’s the catch: not all moisturizers work the same. Lotions with water as the first ingredient evaporate quickly. Ointments like petroleum jelly or ceramide-rich creams last longer. Apply them right after a lukewarm bath, while the skin is still damp. Do it twice a day - morning and night. No fragrances. No dyes. No harsh soaps. Just simple, consistent protection.The Dual Allergen Exposure Hypothesis
Here’s where things get surprising. If skin exposure leads to allergies, why does eating peanut early prevent them? The answer lies in the dual allergen exposure hypothesis. When allergens enter through broken skin, the immune system learns to react. When they enter through the gut - especially early and regularly - the immune system learns to tolerate. The landmark LEAP study proved it. Babies with severe eczema and egg allergy, who were at high risk for peanut allergy, were given peanut protein regularly from 4 to 11 months old. By age 5, they were 86% less likely to develop a peanut allergy than those who avoided it. This doesn’t mean you should start feeding peanut butter to every baby with a rash. But for those with severe eczema or known food allergies, early introduction under medical guidance can be life-changing. Talk to your pediatrician. Get tested if needed. Don’t wait until your child has a reaction to act.
It’s Not Just the Skin - The Gut Matters Too
The skin isn’t the only gateway. The gut is too. Research shows that babies who go on to develop multiple allergies often have a different gut microbiome. Their gut bacteria have less ability to produce butyrate - a short-chain fatty acid that calms the immune system. Think of it as the body’s natural anti-inflammatory. This isn’t about probiotics you buy at the store. It’s about how babies are born, fed, and exposed to microbes. Vaginal birth, breastfeeding, and early exposure to diverse environments (like pets or dirt) help build a healthy microbiome. Antibiotics in the first year? They can disrupt it. While we don’t yet have a probiotic pill that can stop the atopic march, we do know that what happens in the gut and on the skin are linked. A healthy gut supports a balanced immune system. A healthy skin barrier reduces the load on that system.Who’s Actually at Risk?
Not every child with eczema will develop asthma. Only about 25% do. So how do you know if your child is in that group? Three things matter most:- Severity of eczema: Babies with moderate to severe eczema are 3-4 times more likely to develop asthma or food allergies.
- Early onset: Eczema appearing before 3 months of age is a stronger predictor than later-onset cases.
- Family history: A parent or sibling with asthma, hay fever, or food allergies increases risk.
What Doesn’t Work (And Why)
There’s a lot of noise out there. “Switch to organic food.” “Stop all dairy.” “Use coconut oil.” None of these are backed by strong evidence for preventing the atopic march. Avoiding allergens during pregnancy or breastfeeding? No benefit. Delaying solids beyond 6 months? May increase risk. Restricting pets? No clear link. The science points to one clear path: protect the skin, introduce allergens early if high-risk, and support gut health naturally. Everything else is distraction.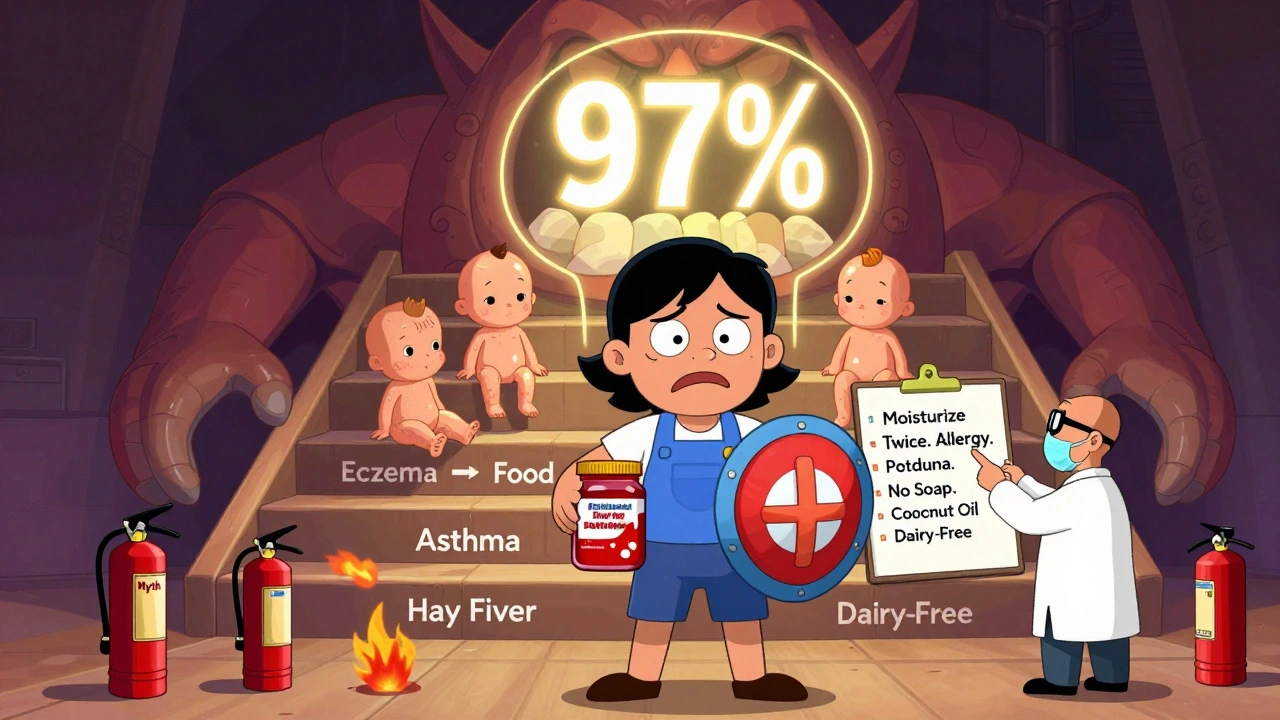
What You Can Do Today
You don’t need a PhD to help your child. Here’s what works:- Start skin care at birth: Use a thick, fragrance-free emollient twice daily - even if there’s no rash yet.
- Use gentle cleansers: No soap. No scrubbing. Just water or a mild, pH-balanced wash.
- Apply moisturizer within 3 minutes of bathing: Lock in moisture while skin is wet.
- For high-risk babies: introduce peanut and egg between 4-6 months, under medical guidance if eczema is severe.
- Avoid triggers: Harsh detergents, hot water, wool, and sweat can worsen eczema. Keep nails short to prevent scratching.
- Watch for signs of asthma: Frequent coughing at night, wheezing with colds, or trouble breathing after play? Talk to your doctor.
It’s Not a Death Sentence
The old idea - that eczema means your child will definitely have asthma - is outdated. Most kids with eczema grow out of it. Many never develop other allergies. But for the ones who might, early action changes everything. Protecting the skin barrier isn’t just about comfort. It’s about giving the immune system a better chance to learn what’s safe. This isn’t about fear. It’s about awareness. You don’t need to fix everything. You just need to know what matters - and act on it.Is eczema the same as allergies?
No. Eczema is a skin condition caused by a combination of genetic and environmental factors, including a defective skin barrier. Allergies are immune responses to specific substances like peanuts or pollen. But eczema often comes first and can lead to allergies because broken skin lets allergens in, triggering the immune system.
Can moisturizing prevent food allergies?
Yes - for high-risk babies. Daily use of thick emollients from birth can reduce the risk of developing eczema by 20-30%. Since eczema is the first step in the atopic march, protecting the skin barrier lowers the chance of allergens entering the body and causing sensitization. This doesn’t guarantee prevention, but it significantly reduces risk.
When should I introduce peanut to my baby?
For babies with severe eczema or egg allergy, introduce peanut-containing foods between 4 and 6 months, under a doctor’s supervision. For babies with mild or no eczema, you can introduce peanut around 6 months along with other solids. Never give whole peanuts - use peanut butter thinned with water or peanut powder mixed into food.
Do I need to avoid certain foods while breastfeeding?
No. Avoiding common allergens like milk, eggs, or nuts during breastfeeding has not been shown to prevent allergies in babies. In fact, early exposure through breast milk may help build tolerance. Focus on a balanced diet and introduce allergens to your baby directly when appropriate.
Will my child outgrow eczema?
Many do. About 60% of children see significant improvement by age 5, and 80% by adolescence. But for those with severe eczema, especially with early onset and family history, symptoms may persist or shift into asthma or allergic rhinitis. Skin care and early intervention can help reduce long-term risk.
Are probiotics helpful for preventing eczema?
Current evidence doesn’t support routine probiotic use for preventing eczema or allergies. While gut health plays a role, specific strains and dosages aren’t yet proven effective for broad prevention. Focus instead on natural ways to support microbiome health: vaginal birth (if possible), breastfeeding, avoiding unnecessary antibiotics, and exposing babies to diverse environments.

Marvin Gordon
December 4, 2025 AT 21:25Just started using petroleum jelly on my 2-month-old twice a day after baths. No more flaky patches. No more midnight scratching. I didn’t believe it at first, but this stuff is basically liquid armor for skin.
Still waiting to introduce peanut butter, but I’m all in on the moisturizing routine now.
Norene Fulwiler
December 6, 2025 AT 03:32I’m a pediatric nurse in Texas and I see this every week. Parents panic about rashes, but they don’t know the difference between dry skin and actual eczema.
Simple rule: if it’s red, cracked, and doesn’t improve with regular lotion - it’s not just dry. It’s a warning sign.
And yes, moisturizing from day one? Game changer. No hype. Just science.
Ada Maklagina
December 7, 2025 AT 01:15Harry Nguyen
December 8, 2025 AT 22:40So let me get this straight - we’re now supposed to believe that slathering baby in Vaseline will prevent the entire modern allergy epidemic?
Next they’ll tell us to duct-tape our kids’ noses to stop hay fever.
Meanwhile, Big Pharma is selling $400 moisturizers while your great-grandma used lard and a prayer.
This is just corporate wellness theater dressed up as science.
James Moore
December 10, 2025 AT 15:28It’s fascinating - and profoundly tragic - that we’ve reached a point in medical discourse where the most effective, low-tech, non-pharmaceutical intervention available - the daily, consistent application of an occlusive emollient - is being elevated to the status of a prophylactic miracle, while the systemic, immunological, and epigenetic underpinnings of atopy are being reduced to a simplistic ‘skin barrier’ narrative.
Yes, filaggrin mutations are critical; yes, early allergen exposure via the gut is protective; yes, the microbiome modulates immune tolerance - but to isolate skin care as the singular lever is not just reductionist, it’s dangerously misleading.
We are not repairing bricks and mortar - we are recalibrating an entire immune system that has been dysregulated by decades of sanitized environments, antibiotic overuse, and processed food diets - and no amount of ceramide cream will undo the consequences of a culture that has lost its connection to soil, sunlight, and microbial diversity.
Moisturize? Yes. But don’t mistake symptom management for root cause resolution.
Kylee Gregory
December 11, 2025 AT 17:05I appreciate how this breaks down the science without fear-mongering.
I used to think my daughter’s eczema was just ‘bad skin’ until I learned about the atopic march.
Now I use the same cream on both kids - one has no issues, the other had severe eczema. The difference isn’t magic - it’s consistency.
And honestly, I think the most powerful thing here is that we don’t have to do everything perfectly. Just do the few things that matter.
One moisturizer at a time, as the post says.
Lucy Kavanagh
December 13, 2025 AT 09:08Did you know the CDC is quietly funding these ‘skin barrier’ studies because they want to replace vaccines with moisturizers?
Think about it - if you convince parents that lotion prevents allergies, they’ll stop vaccinating.
And who benefits? The same companies selling the creams and the formula.
Also, why are all the studies funded by big skincare brands? Coincidence? I think not.
My cousin’s baby had eczema, they used coconut oil and went to a farm in Vermont - no allergies. No creams. No ‘science.’ Just nature.
Trust nature. Not labs.
Chris Brown
December 13, 2025 AT 22:14While the notion of early allergen introduction may appear, on the surface, to be grounded in empirical observation, one must interrogate the ethical and cultural implications of this paradigm.
By encouraging parents to introduce peanut protein at four months - a developmental stage in which the infant’s gastrointestinal and immune systems remain profoundly immature - we are, in effect, engineering an early exposure protocol that prioritizes statistical reduction of allergy incidence over the natural, organic progression of biological maturation.
One might argue that this is proactive medicine. I argue that it is premature intervention - a form of medical hubris that disregards the intrinsic wisdom of developmental timelines.
Moreover, the normalization of such protocols reflects a broader societal trend: the pathologization of childhood vulnerability, and the commodification of parental anxiety.
Let children develop. Let their bodies adapt. Do not intervene - unless absolutely, incontrovertibly necessary.
And even then - proceed with humility.