 Jan, 29 2026
Jan, 29 2026
Graves’ disease isn’t just an overactive thyroid-it’s your immune system turning against you. About 80% of all hyperthyroidism cases in the U.S. come from this condition, where the body mistakenly attacks the thyroid gland, forcing it to pump out too much hormone. This isn’t something you can shake off with rest or caffeine. Left untreated, it can lead to heart rhythm problems, bone loss, and even a life-threatening surge called thyroid storm, which kills 20-30% of those who experience it.
What Actually Happens in Graves’ Disease?
Your thyroid is a small butterfly-shaped gland in your neck. It controls how fast your body uses energy. In Graves’ disease, your immune system produces strange antibodies-called thyroid-stimulating immunoglobulins (TSI)-that latch onto your thyroid like keys in a lock. These keys don’t just open the door; they turn the ignition and keep the engine running nonstop. The result? Too much T3 and T4 hormone flooding your bloodstream. This isn’t random. Women are seven times more likely to get it than men, and most cases show up between ages 30 and 50. If you have a family member with Graves’ or another autoimmune disease like type 1 diabetes or rheumatoid arthritis, your risk jumps. Smoking doesn’t just hurt your lungs-it doubles your chance of developing the eye complications tied to this disease. The classic signs aren’t subtle: rapid heartbeat, trembling hands, weight loss despite eating more, trouble sleeping, and anxiety that feels like your nerves are wired to a live wire. But here’s what many miss: bulging eyes. About half of people with Graves’ develop Graves’ ophthalmopathy-eyes that stare out too far, feel gritty, or become red and swollen. In 3-5% of cases, vision is at risk from pressure on the optic nerve. Even rarer is skin thickening on the shins, called pretibial myxedema, affecting less than 2%.How Do Doctors Confirm It?
It’s not just about symptoms. Blood tests tell the real story. A suppressed TSH (below 0.4 mIU/L) with high free T4 (above 1.8 ng/dL) and free T3 (above 4.2 pg/mL) is the fingerprint of Graves’. But the gold standard is the TRAb test-measuring those rogue antibodies. It’s 95% accurate at confirming the diagnosis. If your TRAb levels are over 10 IU/L, you have an 80% chance of relapse after stopping medication. Doctors also check for eye changes with imaging like CT or MRI scans, especially if you have double vision or pain behind the eyes. Sometimes, a radioactive iodine uptake test is used to see how aggressively the thyroid is grabbing iodine-Graves’ patients typically show high uptake across the whole gland, unlike other thyroid issues where uptake is patchy.Why PTU? The Role of Propylthiouracil in Treatment
The first line of defense is usually antithyroid drugs. Methimazole is the go-to for most adults-it works well, needs just one dose a day, and has fewer serious side effects. But PTU (propylthiouracil) has a critical niche: pregnancy. In the first trimester, methimazole carries a small risk of birth defects. PTU doesn’t cross the placenta as easily, making it the safer choice during early pregnancy. That’s why doctors prescribe it even though it’s riskier overall. PTU can cause severe liver damage in 0.2-0.5% of users-rare, but deadly. That’s why monthly liver function tests are mandatory. One patient shared on a forum: “PTU saved my pregnancy, but the constant blood draws for ALT levels were exhausting. At week 24, mine spiked to 120 U/L. Normal is under 40.” Dosing starts at 100-150 mg three times daily for moderate cases, up to 800 mg daily in severe cases or thyroid storm. As hormone levels drop, the dose is slowly lowered. Most people feel better within weeks, but full control takes months. You’re not done after symptoms fade. Treatment usually lasts 12-18 months to give the immune system a chance to reset.
PTU vs. Methimazole: The Trade-Offs
| Feature | PTU (Propylthiouracil) | Methimazole |
|---|---|---|
| Dosing frequency | Three times daily | Once daily |
| Onset of action | Faster (hours) | Slower (days) |
| Best for | First trimester pregnancy, thyroid storm | Most non-pregnant adults |
| Major risk | Liver toxicity (0.2-0.5%) | Skin reactions (0.1-0.3%), birth defects (if used in early pregnancy) |
| Monitoring required | Monthly liver tests, CBC | CBC every 1-3 months |
| Cost (monthly) | $10-$30 | $10-$25 |
PTU works faster, which is why it’s used in thyroid storm-the medical emergency where your body overheats, your heart races over 140 bpm, and you can slip into coma. But for most people, methimazole is the smarter long-term pick. The liver risk with PTU is low, but it’s not worth taking unless you absolutely need to.
What Happens If Drugs Don’t Work?
About half of people go into remission after 12-18 months of antithyroid drugs. The other half relapse. When that happens, doctors move to one of two permanent options: radioactive iodine or surgery. Radioactive iodine (I-131) is swallowed as a pill. It destroys thyroid tissue over weeks to months. Eighty to ninety percent of patients are cured with one dose. But the trade-off? You’ll almost certainly become hypothyroid and need lifelong thyroid hormone replacement. It’s not a cure-it’s a controlled shutdown. Thyroidectomy removes the gland entirely. It works in 95% of cases, with immediate results. But surgery comes with risks: damage to the voice box (1%) or parathyroid glands (1-2%), which control calcium. If those are hurt, you’ll need calcium supplements for life. Cost-wise, drugs are cheap-$10 to $50 a month. Radioactive iodine runs $300 to $1,500. Surgery? $5,000 to $15,000. Insurance usually covers all three, but out-of-pocket costs vary.Eye Problems Don’t Disappear With Normal Hormones
Here’s the hard truth: even when your TSH and T4 are perfect, your eyes might still bulge, ache, or feel dry. That’s because Graves’ ophthalmopathy is driven by immune cells in the eye socket-not thyroid hormones. So fixing the thyroid doesn’t fix the eyes. For moderate to severe cases, doctors now use intravenous steroids like methylprednisolone. If that doesn’t help after 3-6 months, orbital radiation therapy can reduce swelling in 60-70% of cases. And since 2021, there’s a new drug-teprotumumab-that targets the root cause in the eye tissue. In trials, it reduced bulging eyes by 71%. But it costs $150,000 per course and requires weekly infusions for 6 months. Most insurance requires failure of steroids first.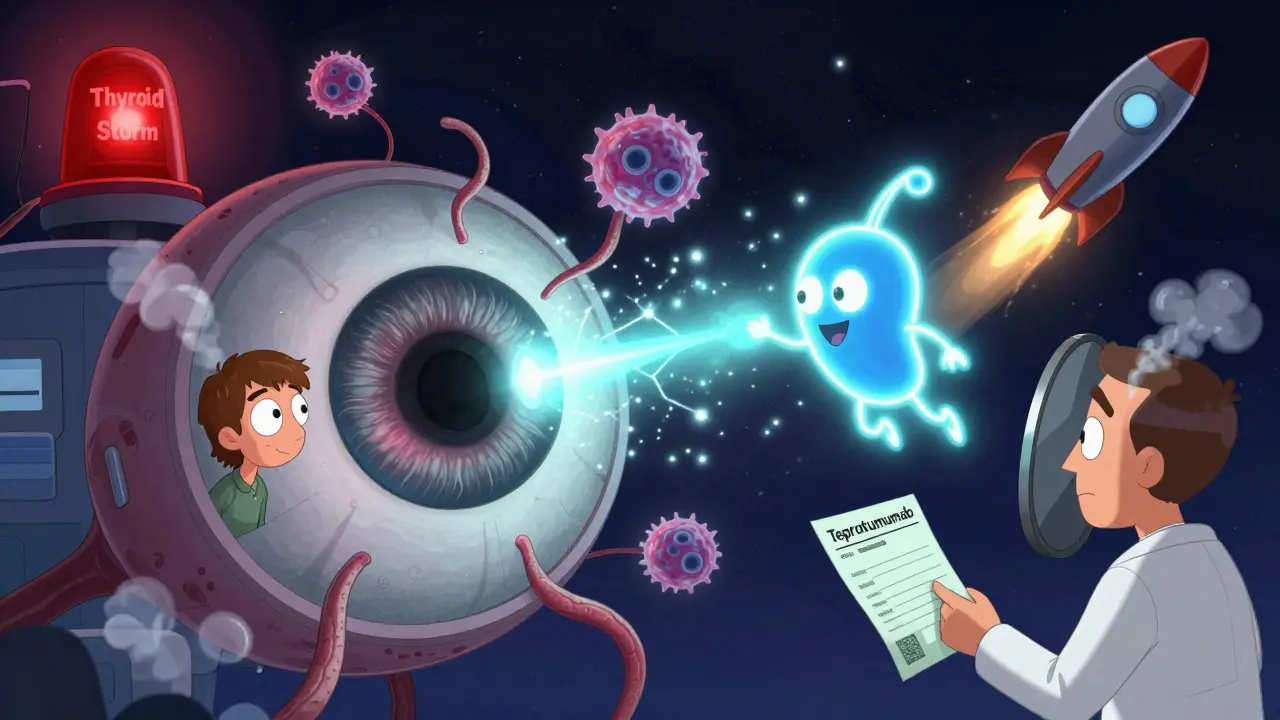
Life After Diagnosis
Many people feel like they’ve been hit by a truck. Anxiety, insomnia, and weight loss are common before diagnosis. One survey found 78% of patients had severe anxiety, and 65% lost 15-20 pounds without trying. Diagnosis delays are common-42% of patients wait 6 to 12 months because doctors mistake symptoms for stress, depression, or menopause. Once treatment starts, most reach normal hormone levels within three months. But managing it is a marathon. You need regular blood tests. You need to recognize signs of too much medication-like feeling cold, tired, or gaining weight-which means you’re now hypothyroid from over-treatment. Heart rate above 100 bpm or fever over 100.4°F? Call your doctor immediately. Support matters. The Graves’ Disease and Thyroid Foundation runs a 24/7 helpline. Online communities like Reddit’s r/GravesDisease have over 12,500 members sharing tips, frustrations, and wins. One person wrote: “I thought I was just anxious. Turns out, my body was on fire.”What’s Next for Graves’ Disease?
Science is moving fast. In 2022, the FDA approved the first home thyroid monitor-ThyroidTrack-that lets you check TSH with a finger-prick device. It’s still in research use, but it’s coming. Clinical trials are testing drugs that block the TSH receptor directly, with early results showing 85% of patients normalizing without becoming hypothyroid. B-cell therapies like rituximab, used in rheumatoid arthritis, are showing promise in resistant cases. And researchers are now using genetic markers-like HLA-DR3-to predict who’s more likely to relapse. The NIH just launched a $12.5 million project to build personalized treatment plans based on your immune profile. PTU won’t disappear. Even with its risks, it’s still the only safe option for early pregnancy. Experts predict it’ll remain in use for 15-20% of Graves’ patients through 2030. It’s not perfect-but for some, it’s the only lifeline.Frequently Asked Questions
Can Graves’ disease be cured?
Graves’ disease can go into remission, especially after 12-18 months of antithyroid drugs. About 30-50% of people stop treatment and never relapse. But for many, the immune system eventually restarts the attack. Permanent treatments like radioactive iodine or surgery remove the thyroid entirely, which ends the overactivity but requires lifelong hormone replacement. So while the disease can be controlled, true cure depends on how you define it.
Is PTU safe during pregnancy?
PTU is the preferred antithyroid drug during the first trimester because it crosses the placenta less than methimazole, lowering the risk of birth defects. But it carries a small risk of severe liver damage in the mother. Doctors monitor liver enzymes monthly. After the first trimester, most switch back to methimazole because the baby’s organs are formed and PTU’s liver risks outweigh its benefits.
Why do I still have eye symptoms after my thyroid levels are normal?
Graves’ eye disease is caused by immune cells attacking tissue behind the eyes-not by thyroid hormone levels. That’s why fixing your thyroid doesn’t fix your eyes. Treatments like IV steroids, orbital radiation, or the drug teprotumumab target the inflammation in the eye socket directly. You may need to see an ophthalmologist who specializes in thyroid eye disease for the best results.
Can smoking make Graves’ disease worse?
Yes. Smoking doubles your risk of developing Graves’ ophthalmopathy and makes existing eye problems much worse. It also reduces the effectiveness of treatments like steroids and radiation. Quitting smoking isn’t just a good idea-it’s a medical necessity if you have Graves’ disease.
What are the signs of a thyroid storm?
Thyroid storm is a medical emergency. Signs include a fever above 101.3°F, heart rate over 140 bpm, confusion, vomiting, diarrhea, and extreme weakness. It can lead to heart failure, seizures, or coma. If you have Graves’ disease and suddenly feel this bad, call 911 or go to the ER immediately. It’s rare but deadly-20-30% of cases are fatal without urgent treatment.
