 Feb, 11 2026
Feb, 11 2026
For decades, hepatitis C was a slow-moving crisis - a silent infection that damaged the liver for years before anyone knew it was there. Back then, treatment meant weekly injections, brutal side effects, and a coin flip at best for a cure. Today, that’s all changed. With direct-acting antivirals (DAAs), more than 95% of people with hepatitis C can be cured in just 8 to 12 weeks - with no shots, no hospital visits, and almost no side effects. This isn’t science fiction. It’s real, and it’s happening right now.
How DAAs Changed Everything
Before DAAs, hepatitis C treatment relied on interferon and ribavirin. These drugs didn’t target the virus directly. Instead, they tried to boost the body’s immune system to fight it off. The result? A 40% to 60% cure rate, along with fatigue, depression, anemia, and flu-like symptoms that made daily life impossible for many. Treatment lasted up to 48 weeks. Many patients quit because it was too hard to endure.
Then came sofosbuvir (Sovaldi) in late 2013. It was the first true DAA - a pill that blocked a key protein the hepatitis C virus needed to copy itself. Within months, new combinations followed: glecaprevir-pibrentasvir, sofosbuvir-velpatasvir, sofosbuvir-velpatasvir-voxilaprevir. These are called pangenotypic regimens because they work against all major strains of the virus. No more testing for genotype 1a vs 3b. Just one pill, once a day, for 8 to 12 weeks.
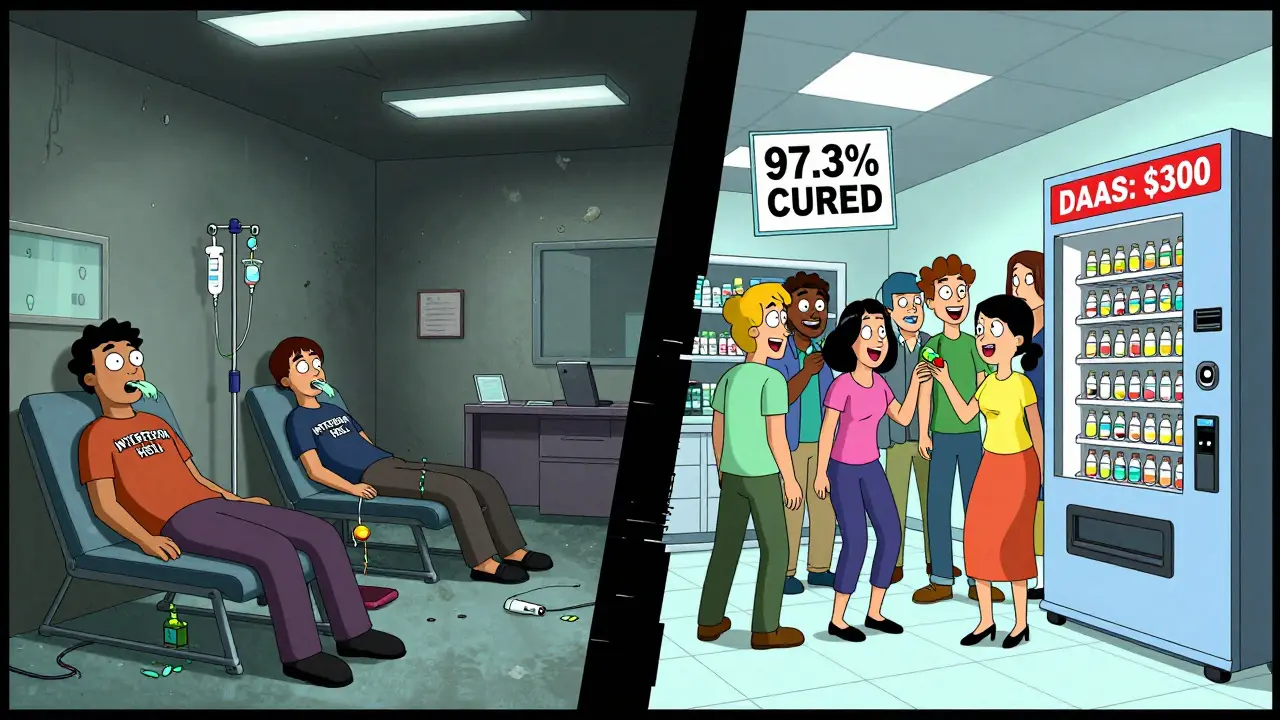
The numbers speak for themselves. A U.S. study of over 6,600 insured patients treated between 2014 and 2021 found that 97.3% achieved a sustained virologic response (SVR) - meaning the virus was undetectable 12 weeks after treatment ended. That’s the medical definition of cured. Another study of 238 real-world patients showed 92.8% cure rates. Even in people with HIV and hepatitis C coinfection, cure rates matched those of people with hepatitis C alone.
Cure Rates Across Different Groups
DAAs work well for almost everyone - but not equally well for everyone.
People without cirrhosis (early-stage liver damage) have the highest cure rates: around 96.7% with sofosbuvir-velpatasvir. That’s nearly perfect. But for those with advanced cirrhosis - where the liver is already scarred and struggling - the cure rate drops to about 87.1%. Still impressive, but it shows that damage done before treatment matters.
Here’s the troubling part: patients with decompensated cirrhosis (liver failure) or liver cancer (HCC) are 30% less likely to get treated. Why? Some doctors think they’re too sick. Others worry about drug interactions. But research shows curing hepatitis C in these patients improves survival, reduces hospital stays, and even helps with liver transplant outcomes. Yet, they’re often left behind.
Age, race, and income don’t affect how well DAAs work - but they do affect who gets access. A U.S. study found that Medicaid patients were only 23% likely to get treated within a year of diagnosis. That’s one in four. In contrast, patients with private insurance had treatment rates closer to 70%. The Northeast and Midwest had 20-30% higher treatment rates than the West, even after adjusting for income and education. This isn’t about medical effectiveness. It’s about systems failing people.
Why Cure Matters Beyond the Liver
Getting rid of hepatitis C isn’t just about saving the liver. It’s about saving your whole body.
Before DAAs, people with hepatitis C had a much higher risk of kidney disease, diabetes, heart problems, and even certain cancers. A 2023 study in JAMA Network Open showed that people who were cured had 30% fewer cases of chronic kidney disease and end-stage kidney failure compared to those who never got treated. That’s not a small difference - it’s life-changing.
Cure also reduces inflammation. Hepatitis C doesn’t just sit in the liver. It triggers a low-grade, long-term immune response that damages blood vessels, kidneys, and even the brain. When the virus is gone, that inflammation drops. Many patients report feeling more energy, less brain fog, and fewer joint aches within months of treatment.
And here’s something many don’t realize: curing hepatitis C cuts death risk. A 2024 study estimated that if we treat everyone who needs it, we could prevent 456,000 HCV-related deaths in the U.S. alone between 2014 and 2030. Without treatment, that number climbs to over 770,000.
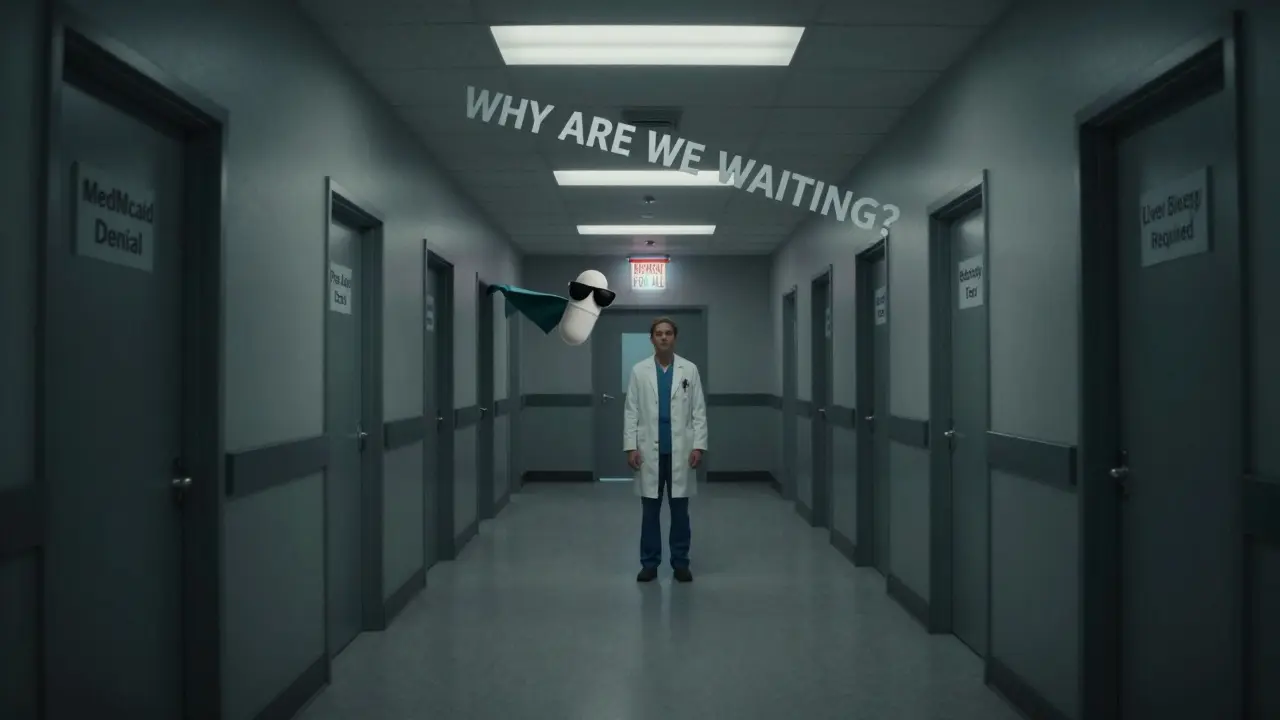
The Access Problem: Why So Few Get Treated
Here’s the harsh truth: we have the cure. But we’re not giving it to everyone who needs it.
When DAAs first launched in 2013, a 12-week course cost $84,000. That price scared insurers, governments, and patients alike. But prices have dropped sharply. Generic versions now cost between $260 and $2,800 per course depending on the country. In Australia, Canada, and parts of Europe, treatment is covered by public health systems. In the U.S., many state Medicaid programs still require prior authorizations, liver biopsy proof, or sobriety requirements - rules that don’t exist for diabetes or high blood pressure.
Global access is even more uneven. While 91% of countries have registered at least one DAA, only 68% provide reimbursement. In low- and middle-income countries, 52% don’t cover any DAA therapy. And in 61% of countries with reimbursement, only specialists can prescribe them - meaning rural patients, prisoners, or homeless people have almost no access.
The COVID-19 pandemic made things worse. Clinic visits dropped. Screening programs were paused. People with hepatitis C slipped through the cracks. By 2020, only 65.2% of diagnosed, viremic patients in the U.S. received treatment - down from previous years. The momentum stalled.
What’s Next? The Path to Elimination
The World Health Organization wants to eliminate hepatitis C as a public health threat by 2030. That means 90% fewer new infections and 65% fewer deaths. We’re not on track.
The tools are here. We have pills that cure 95%+ of people. We have tests that detect the virus with a simple blood draw. We have guidelines that say primary care doctors - not just liver specialists - can manage most cases.
So why isn’t it happening?
Because we still treat hepatitis C like it’s a punishment, not a medical condition. We make people jump through hoops. We wait until their liver is failing before we act. We forget that people who use drugs, who are homeless, who are incarcerated - they deserve treatment too.
Real progress means changing systems, not just prescribing pills. It means integrating hepatitis C screening into routine care: at ERs, in drug treatment centers, in prisons, in primary care clinics. It means removing prior authorizations and income-based barriers. It means treating hepatitis C like we treat hypertension - early, easy, and everywhere.
There’s hope. In Australia, where DAAs are fully funded and available without restrictions, treatment rates jumped from 5% to over 70% in just five years. The number of new infections has dropped by 80%. We can do this. But only if we stop treating access as an afterthought.
What You Should Do
If you’ve ever had a blood transfusion before 1992, used injection drugs, gotten a tattoo in an unregulated setting, or were born between 1945 and 1965 - get tested. One blood test. No fasting. No needles. Just a quick finger prick or vein draw.
If you’re diagnosed: don’t wait. DAAs are simple, effective, and safe. Ask your doctor for a pangenotypic regimen like glecaprevir-pibrentasvir or sofosbuvir-velpatasvir. If your insurance denies it, appeal. There are patient assistance programs. Nonprofits. Pharmacies that offer discounts. You don’t have to pay $80,000. You can get cured for under $300 in many places.
If you’re a healthcare provider: stop waiting for liver specialists. Start testing. Start treating. You don’t need a liver biopsy. You don’t need to be an expert. Just follow the guidelines. The cure is in the pill.
Hepatitis C is no longer a death sentence. It’s a solvable problem. But solving it isn’t about science. It’s about will.
What does "cured" mean in hepatitis C treatment?
Being cured means the hepatitis C virus is no longer detectable in your blood 12 weeks after finishing treatment. This is called a sustained virologic response (SVR). Once you reach SVR, the virus is gone for good - you can’t pass it on, and your risk of liver damage, cancer, or death drops dramatically. It’s not a temporary fix. It’s a permanent cure.
Can you get hepatitis C again after being cured?
Yes. Being cured doesn’t give you immunity. If you’re exposed again - through sharing needles, unsterile tattoos, or unprotected sex with an infected person - you can get infected again. That’s why ongoing prevention matters. Even after cure, avoid risky behaviors. Regular testing is still recommended if you’re at ongoing risk.
Do DAAs work for people with cirrhosis or liver cancer?
Yes, but the cure rate is lower. For people with cirrhosis, cure rates drop to about 87%, compared to 97% in those without liver damage. Even so, curing the virus improves survival, reduces the chance of liver failure, and can make liver transplant more successful. People with liver cancer (HCC) can still be treated - but many don’t get the chance due to outdated guidelines or provider bias. New evidence shows they benefit the most.
How long does DAA treatment take?
Most DAA regimens last 8 to 12 weeks. Some patients with advanced cirrhosis or prior treatment failure may need 24 weeks. But for the vast majority, it’s a once-daily pill for three months. No injections. No weekly clinic visits. Just take the pills as directed and get tested 12 weeks after finishing.
Are generic DAAs as effective as brand-name ones?
Yes. Generic versions of sofosbuvir, velpatasvir, and glecaprevir-pibrentasvir are bioequivalent to brand-name drugs. They contain the same active ingredients, work the same way, and have the same cure rates - over 95%. The only difference is cost. In many countries, generics cost under $300 per course. In the U.S., some programs offer them for under $500. There’s no medical reason to choose the expensive brand.
Why aren’t more people getting treated if DAAs are so effective?
The biggest barrier is access, not effectiveness. Many people don’t know they’re infected. Others can’t afford treatment, even with insurance. Some face bureaucratic hurdles like prior authorizations, mandatory sobriety requirements, or specialist-only prescribing. In the U.S., only 23% of Medicaid recipients get treated within a year of diagnosis. Globally, many low-income countries don’t cover DAAs at all. It’s a system failure - not a medical one.
