 Dec, 1 2025
Dec, 1 2025
Overdose isn’t just a statistic-it’s someone’s parent, sibling, friend, or neighbor. Every day, people die from overdoses because they used a drug they thought was safe, didn’t have access to help, or didn’t know what to do when things went wrong. The truth is, overdose prevention works-but only if we use the right tools, at the right time, and with real compassion.
Know What’s in the Drugs
Most overdose deaths today aren’t from heroin or prescription pills. They’re from fentanyl, a synthetic opioid 50 to 100 times stronger than morphine. It’s mixed into cocaine, meth, counterfeit pills, and even MDMA. People don’t know they’re taking it. That’s where fentanyl test strips come in. These small paper strips cost less than a dollar each. You mix a tiny bit of the substance with water, dip the strip in, and wait a minute. One line means no fentanyl detected. Two lines? Fentanyl is present. It’s not perfect-some tests miss low doses or don’t work with all chemicals-but it’s the best early warning system we have. The CDC says these strips can detect fentanyl at levels as low as 0.25 nanograms. That’s enough to kill. Use them. Always. Even if you’ve used the same source before. Drug supplies change daily. A pill that was safe last week could be deadly this week.Keep Naloxone On Hand
Naloxone (brand names Narcan, Kloxxado) is the only medicine that can reverse an opioid overdose. It’s safe, easy to use, and doesn’t work on non-opioid drugs like cocaine or xylazine. But it saves lives when opioids are involved. The FDA approved the first over-the-counter naloxone nasal spray in March 2023. You don’t need a prescription. You can buy it at pharmacies, community centers, or online. It’s designed for anyone-even someone with no medical training. Here’s how to use it:- Call 911 immediately.
- Check if the person is breathing. If not, give two rescue breaths.
- Place the nozzle in one nostril and press the plunger firmly.
- Wait 2-3 minutes. If no response, give a second dose in the other nostril.
- Stay with them until help arrives.
Medication-Assisted Treatment Works
The single most effective way to prevent overdose is to treat the addiction-not just the overdose. Medication-assisted treatment (MAT) uses FDA-approved drugs: methadone, buprenorphine, and naltrexone. Methadone and buprenorphine reduce cravings and withdrawal. They don’t get you high when taken as prescribed. Naltrexone blocks opioids entirely. All three cut overdose death risk by about 50%, according to the World Health Organization. That’s better than any therapy alone. But here’s the problem: only 18.4% of Americans with opioid use disorder got any medication-based treatment in 2022. In rural areas, 60% of counties have no MAT provider at all. If you or someone you know needs help, don’t wait for the perfect clinic. Call SAMHSA’s helpline (1-800-662-HELP). They’ll connect you to providers-even if it’s a telehealth appointment.Never Use Alone
Most overdoses happen alone. People hide their use out of shame, fear, or isolation. But using alone is the biggest risk factor. The “Never Use Alone” hotline lets you call someone before you use. They stay on the line while you do. If you stop responding, they call 911 and send help. In 2023, they responded to 12,000 overdose incidents per month. That’s 360,000 lives potentially saved in a year. You don’t need to be “addicted” to use this service. You don’t need to be in recovery. You just need to be alive. If you’re using alone, call them. Or better yet-use with someone who has naloxone and knows how to use it.
Build a Safety Plan
A safety plan isn’t just for suicide prevention. It works for overdose too. The New York State Department of Health found people who used a structured safety plan had 28% fewer overdose events. Here’s how to build one:- Who will you call before you use? (A friend, hotline, family member)
- Where will you use? (Safe, not alone, not in bed)
- Do you have naloxone? (Keep it with you)
- Do you know how to use it? (Practice with a trainer or video)
- What’s your exit plan if things go wrong?
Know the New Threats
Fentanyl isn’t the only danger anymore. Xylazine, a veterinary sedative, is now showing up in street drugs. It’s not an opioid. Naloxone won’t reverse it. It causes severe skin ulcers, slow breathing, and deep sedation. The DEA found it in 23% of fentanyl powder and 7% of fentanyl pills seized in 2022. If someone is unresponsive, has shallow breathing, or looks unusually pale or cold, treat it like an overdose anyway. Give naloxone anyway-it won’t hurt, and it might help if opioids are mixed in. Call 911. Stay with them. Even if naloxone doesn’t fully wake them, medical help can still save their life.Help After Release from Jail or Prison
People released from incarceration are 120 times more likely to die of overdose in the first two weeks. Why? Their tolerance drops fast. They go back to using the same dose they used before jail. Their body can’t handle it. The CDC and SAMHSA now recommend giving naloxone and starting MAT before release. If you or someone you know is getting out of jail, ask for help before leaving. Bring your safety plan. Get naloxone. Connect with a community health worker. Don’t rely on luck.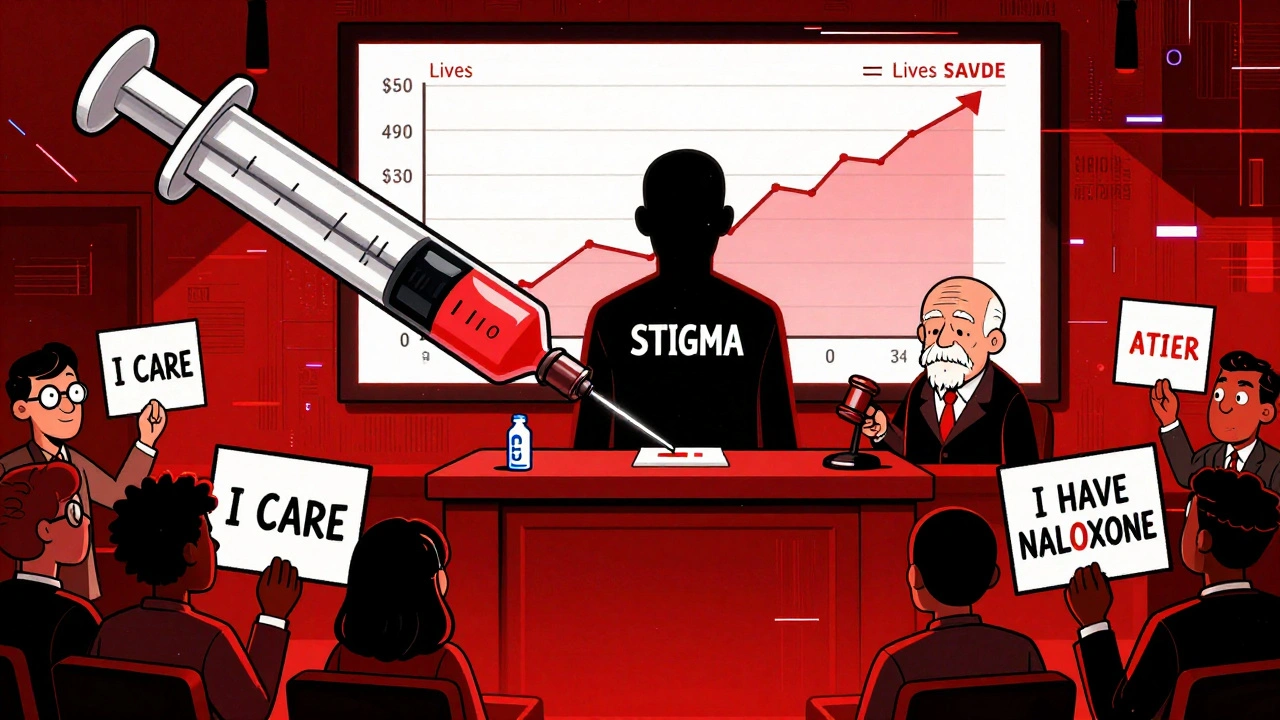
Reduce the Stigma
Stigma kills. It stops people from calling 911. It keeps them from asking for naloxone. It makes them feel like they don’t deserve help. If you’re a friend, family member, or coworker, say this: “I care about you. I want you to be safe.” Don’t judge. Don’t lecture. Don’t wait for them to “hit rock bottom.” Rock bottom is often a funeral. Offer naloxone. Ask if they’ve used fentanyl test strips. Suggest the Never Use Alone hotline. You don’t need to fix their life. You just need to be someone who shows up.What to Do If You See an Overdose
You don’t need to be a medic. You just need to act. 1. Check responsiveness. Shake gently. Shout their name. No response? Move to step two. 2. Call 911. Say: “Someone is not breathing. I think it’s an overdose.” 3. Give naloxone. Use the nasal spray. One dose in each nostril if needed. 4. Give rescue breaths. Tilt head back, pinch nose, give one breath every 5 seconds. 5. Stay until help arrives. Even if they wake up, they can relapse into overdose. Naloxone wears off faster than opioids. 6. Don’t leave them alone. Even if they say they’re fine. Monitor breathing for at least 2 hours.Where to Get Help
You don’t have to do this alone.- Naloxone: Available at most pharmacies without a prescription. Many community health centers give it out for free.
- Fentanyl test strips: Available through harm reduction organizations like Dances with Drugs, DanceSafe, or local syringe services.
- Medication-assisted treatment: Call SAMHSA’s helpline at 1-800-662-HELP (4357). They’ll find providers near you.
- Never Use Alone: Call 1-800-484-3731 or text 1-800-484-3731. Available 24/7.
- MyNarcan app: Free app that shows nearby naloxone locations and guides you through overdose response.

Shannara Jenkins
December 2, 2025 AT 12:07Just picked up a pack of test strips and two naloxone kits at the pharmacy today-no prescription, no hassle. Seriously, if you’re even a little bit curious about harm reduction, just do it. It’s cheaper than a coffee and could save someone’s life. I keep one in my purse and one in my car. No shame in being prepared.
Also, the Never Use Alone hotline? I told three friends about it this week. One of them actually called it last night. That’s the kind of ripple effect we need.
Alicia Marks
December 4, 2025 AT 06:03Carry naloxone. Period.
Jay Everett
December 5, 2025 AT 06:36Bro. I used to think harm reduction was enabling. Then my cousin OD’d in his apartment and the only thing that brought him back was a stranger’s naloxone. That dude didn’t even know his name. He just saw him blue and acted.
Now I carry two Narcan sprays, test strips in my wallet, and I’ve taught my whole crew how to do rescue breaths. It’s not about judging people-it’s about refusing to let them die because we were too scared to talk about it.
Also, xylazine is a nightmare. My buddy got a wound that looked like a burn from a cigarette but it was just from a drug hit. No opioids involved. Naloxone did jack. He’s lucky he got to the ER in time.
Stop waiting for someone to ‘hit rock bottom.’ Rock bottom is a morgue drawer. Be the person who shows up before the fall.
And yeah, I’m crying while typing this. So what? I’d rather be emotional than empty-handed when it matters.
Elizabeth Grace
December 5, 2025 AT 10:58Okay but like… why does it feel like the only people who care about this are the ones who’ve lost someone? I get it, grief is powerful. But shouldn’t we be doing this before the funeral? I just don’t get why we wait until it’s too late to act.
Also, I used to think people who used drugs were ‘weak.’ Now I just feel angry at how broken the system is. You don’t get MAT unless you’re rich or lucky. That’s not a choice. That’s a trap.
Rebecca M.
December 7, 2025 AT 09:58So let me get this straight-we’re giving out free naloxone like it’s candy, but we won’t give someone a job or housing? How about we stop treating addiction like a medical emergency and start treating poverty like one?
Also, ‘Never Use Alone’ sounds cute, but if you’re using alone, you’re probably also homeless, unemployed, and terrified. No amount of hotline numbers fixes that.
Just saying. Maybe the real harm reduction is… not making people feel like they have to hide to survive?
Steve Enck
December 8, 2025 AT 17:49While the empirical data on naloxone distribution and fentanyl test strips is statistically significant, one must interrogate the underlying ontological assumptions of harm reduction ideology. Is the goal to preserve life at all costs, or to perpetuate a cycle of dependency by decoupling consequence from behavior?
One cannot deny the empirical efficacy of these interventions-but one must also confront the metaphysical paradox: if we remove the risk of death, do we inadvertently remove the impetus for transformation?
It is not compassion that saves; it is accountability. And accountability, by its very nature, requires discomfort. We have mistaken comfort for care.
Let us not mistake the suppression of symptoms for the cure of disease.
Paul Keller
December 9, 2025 AT 22:55Steve, you’re talking like a tenured professor who’s never held a fentanyl test strip in his hand. You think accountability means letting people die so they ‘learn their lesson’? That’s not philosophy-that’s cruelty wrapped in jargon.
I’ve worked in ERs for 17 years. I’ve seen the same guy OD three times. Each time, we brought him back. The fourth time, he asked for buprenorphine. He’s been clean for 14 months now. He works at a bike shop. He’s engaged.
He didn’t ‘transform’ because he almost died. He transformed because someone gave him a chance without judgment. That’s what MAT and naloxone do-they buy time. And time? Time is the only thing that lets someone choose to change.
So no, I don’t need to ‘interrogate the ontology’ of saving lives. I just need to keep my Narcan charged and my heart open.
Laura Baur
December 10, 2025 AT 10:07Paul, your anecdote is emotionally compelling, but it is not evidence-based policy. The CDC’s own data shows that MAT adherence rates remain below 20% even in urban centers with robust access. The root issue is not stigma-it is the failure of the healthcare system to integrate behavioral health into primary care.
Furthermore, the proliferation of test strips has not correlated with a significant decline in overdose mortality in states with the highest distribution rates. This suggests a phenomenon of substitution: users feel falsely secure, and thus engage in riskier behaviors.
One must question whether harm reduction, as currently implemented, is a palliative or a preventative strategy. The former is compassionate. The latter requires structural reform-not band-aids.
Roger Leiton
December 10, 2025 AT 22:06Hey Laura, I get what you’re saying about structural stuff-but I’ve seen people get their first dose of buprenorphine and cry because no one ever told them they could feel normal again. That’s not a band-aid. That’s a lifeline.
And yeah, maybe test strips don’t stop every death. But they stopped one for my cousin. And that one? That one mattered.
Also, I just downloaded MyNarcan. It found a free kit 3 blocks from my apartment. I’m keeping it in my glovebox now. 😊
Maybe the system’s broken. But I’m not waiting for it to fix itself before I do something. I’ve got two sprays. I’ve got strips. I’ve got a friend who calls me before he uses. That’s my contribution.
And honestly? I’ll take imperfect action over perfect silence any day.
Lynn Steiner
December 12, 2025 AT 03:55Why are we always talking about drugs? What about the real problem? The drugs are coming from Mexico. The cartels are poisoning our kids. We need to build the wall, not hand out test strips.
And why is everyone so nice to addicts? I work 60 hours a week and I can’t even get a prescription for my back pain. But they give free Narcan to people who choose to ruin their lives?
It’s not fair. And it’s not right. 😡