 Jan, 20 2026
Jan, 20 2026
Getting the right dose of liquid medicine isn’t just about following instructions-it’s about survival. A single mistake in reading a label can mean giving your child five times too much medicine-or not enough. In the U.S., over 1.3 million injuries each year come from medication errors, and nearly half of them involve liquid prescriptions. The good news? You don’t need a medical degree to read these labels correctly. You just need to know what to look for-and what to ignore.
Milliliters Only: The One Unit That Matters
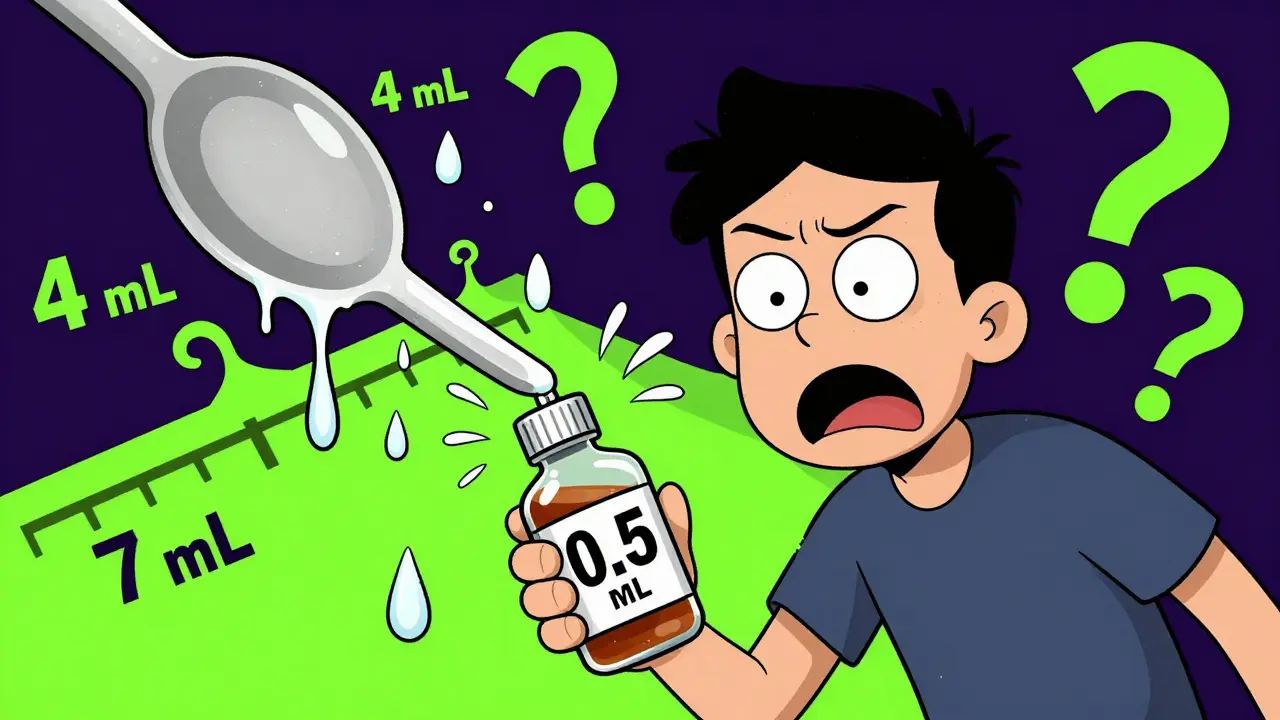
Look at any modern liquid prescription label. You’ll see one unit: mL. That’s milliliters. Not teaspoons. Not tablespoons. Not drops. Just mL.This isn’t a suggestion. It’s a rule. Since 2016, the FDA and the National Council for Prescription Drug Programs (NCPDP) have required all pharmacies to use milliliters on liquid medication labels. Why? Because household spoons are wildly unreliable. A teaspoon from your kitchen might hold 4 mL one day and 7 mL the next. That’s a 75% difference. For a baby on a 0.8 mL dose, that’s life or death.
Pharmacies that still use tsp or tbsp on labels are breaking federal guidelines. If you see it, ask for a corrected label. Most major chains like CVS, Walgreens, and Rite Aid follow this rule. Independent pharmacies? Less consistent. But you have the right to demand clarity.
Decimals Are Not Optional: 0.5 mL, Not .5 mL
Look at the number before the mL. Is it written as 0.5 mL? Good. Is it written as .5 mL? That’s dangerous.That tiny zero before the decimal point saves lives. In 2018, a Johns Hopkins study found that removing leading zeros caused 10-fold dosing errors-like giving 5 mL instead of 0.5 mL-in 47% of cases. That’s not a typo. That’s a fatal mistake. Always check: if the dose is less than 1 mL, it must start with a zero. No exceptions.
And never trust a label that says 5.0 mL. That trailing zero after the decimal is also banned under safety standards. It makes people think precision matters more than it does. The correct form is always 5 mL.
Concentration: What You’re Actually Getting
The label doesn’t just say how much to take-it says how strong the medicine is. That’s the concentration. You’ll see it written like this: 125 mg / 5 mL.This means: every 5 milliliters of liquid contains 125 milligrams of the active drug. If your prescription says to give 10 mL, you’re giving two doses of 125 mg-so 250 mg total. If you only need 125 mg, you give 5 mL.
People often confuse the concentration with the total volume. The bottle might say 100 mL on the side. That’s how much medicine is in the whole bottle-not how much to give at once. Always focus on the dose instruction: “Take 5 mL”-not the total bottle size.

The Dosing Device: Never Use a Kitchen Spoon
The pharmacy should give you a dosing tool: a syringe, a cup with mL markings, or a dropper. Use it. Every time.Even if the label says “1 teaspoon,” don’t grab your kitchen spoon. That’s how most errors happen. A 2019 Consumer Reports study found that 83% of household teaspoons hold more than 5 mL. Some hold up to 7.5 mL. That’s 50% too much.
Use the tool that came with the medicine. If it didn’t come with one, ask the pharmacist for a free oral syringe. They’re small, accurate, and easy to use. For babies, a 1 mL or 5 mL syringe works best. For older kids, a dosing cup with bold mL lines is ideal.
Pro tip: Always draw up the dose slowly. If you’re using a syringe, pull the plunger to the exact line. Don’t guess. If the medicine drips, you’ve gone too far. Start over.
What to Do If the Label Is Confusing
Sometimes, even with all the rules, labels are messy. Maybe the font is too small. Maybe the concentration is printed in tiny text. Maybe the dose instruction says “give every 6 hours” but doesn’t say how many days.Don’t guess. Call the pharmacy. Ask: “Can you confirm the dose? I want to make sure I’m giving the right amount.”
Pharmacists are trained to explain this. They’ve seen hundreds of parents panic over the same confusion. There’s no such thing as a dumb question. In fact, the American Society of Health-System Pharmacists says the “teach-back” method-where you repeat the instructions back to them-is the most effective way to prevent errors. If you can explain how to give the dose in your own words, you’re safe.
Common Mistakes (And How to Avoid Them)
- Mistake: Thinking the total bottle volume is the dose. Fix: Ignore the “100 mL” on the bottle. Only look at “Take 5 mL.”
- Mistake: Using a regular spoon because “it’s close enough.” Fix: Always use the dosing tool. Even if it’s inconvenient.
- Mistake: Assuming 1 tsp = 5 mL. Fix: Even if you know the conversion, don’t trust your spoon. Use the syringe.
- Mistake: Giving the same dose for multiple days without checking the expiration. Fix: Check the expiration date on the label. Most liquid medicines expire in 14 days after opening.

Why This Matters More for Kids
Children under 12 get 75% of all liquid prescriptions. Their bodies are smaller. A tiny mistake can be huge. That’s why the American Academy of Pediatrics pushed hard for these standards.Studies show that when parents get clear labels and a demonstration from the pharmacist, error rates drop from 39% to just 8%. That’s a 78% improvement. The difference isn’t just in the label-it’s in the conversation.
Ask the pharmacist: “Can you show me how to give this?” Watch them. Then do it yourself in front of them. If you can measure it right on the first try, you’re golden.
What’s Changing in 2026
New rules are coming. In January 2023, NCPDP updated its standards to require higher contrast printing and minimum 10-point font size for critical info. The FDA is also testing pictograms-simple pictures showing how to use a syringe-on labels. Early tests show they reduce errors by 37%.Some pharmacies, like Amazon Pharmacy and Medly, are already adding QR codes to labels. Scan it, and you’ll see a 30-second video showing exactly how to measure the dose. It’s not everywhere yet-but it’s coming fast.
By 2026, full compliance is expected across all U.S. pharmacies. But until then, you’re your child’s best defense. Know the rules. Ask questions. Use the right tool. Never assume.
Final Check: The 5-Second Label Test
Before you give any liquid medicine, do this:- Find the dose: Is it in mL? (If not, return it.)
- Check the number: Does it have a leading zero if under 1? (0.3 mL, not .3 mL.)
- Find the concentration: Is it written as “X mg / 5 mL”?
- Use the right tool: Did you get a syringe or dosing cup?
- Confirm: Can you explain this dose to someone else without looking?
If you answered yes to all five, you’re safe. If any answer is no-stop. Call the pharmacy. Don’t risk it.
Medication safety isn’t about being perfect. It’s about being careful. And with these simple steps, you’re already ahead of 80% of people who give liquid medicine at home.
Can I use a kitchen spoon if I don’t have a dosing cup?
No. Household spoons vary too much in size-some hold 4 mL, others hold 8 mL. That’s a 100% difference. Even if you think your spoon is accurate, it’s not. Always use the dosing tool provided by the pharmacy. If you lost it, call them for a free replacement. They’re required to give you one.
What if the label says ‘1 tsp’ instead of ‘5 mL’?
That label is outdated and unsafe. By federal guidelines, it should say ‘5 mL.’ Take the medicine back to the pharmacy and ask them to re-label it. Most will do it immediately. If they refuse, ask to speak to the pharmacist-in-charge. This is a known safety violation.
How do I know if I’m giving too much or too little?
Check the concentration. If the label says ‘120 mg / 5 mL’ and you’re supposed to give 10 mL, you’re giving 240 mg total. If your child’s prescription says ‘120 mg every 6 hours,’ then 10 mL is correct. If you’re unsure, call the prescribing doctor or pharmacist. Never rely on memory or guesswork.
Why does the bottle say ‘100 mL’ if I only need to give 5 mL?
That’s the total amount of medicine in the bottle-not the dose. Most liquid medicines come in 100 mL or 200 mL bottles so you have enough for the full course of treatment. You might only need 5 mL per dose, but you’ll take it 3 or 4 times a day for 7-10 days. Always read the dosage instruction separately from the total volume.
Are liquid medicines safe after the expiration date?
No. Most liquid medications expire 14 days after opening, even if the bottle says a later date. The active ingredients can break down, and bacteria can grow. Never use expired liquid medicine. If you have leftover medicine, return it to the pharmacy for safe disposal. Don’t pour it down the drain.

Stephen Rock
January 21, 2026 AT 01:07Milliliters only. That’s it. No more ‘teaspoons.’ If your pharmacy still uses tsp, they’re literally playing Russian roulette with your kid’s life. I’ve seen it. A 0.5 mL dose turned into 5 mL because someone ‘guessed’ with a spoon. Baby went to the ER. No joke. The FDA didn’t make these rules for fun.
And that leading zero? Non-negotiable. .5 mL is a death sentence written in tiny font. I work in pharma compliance. I’ve reviewed hundreds of labels. Half the errors come from missing zeros. It’s not a typo. It’s negligence.
Also-why are people still using kitchen spoons? I get it, you’re tired. You’re up at 3 AM with a feverish kid. But your ‘close enough’ spoon is a 7 mL monster. That’s not ‘close.’ That’s a 40% overdose. Use the syringe. Even if it’s sticky. Even if you hate it. Your child isn’t a lab rat.
And don’t even get me started on expiration dates. Liquid meds go bad faster than milk in July. 14 days. Period. If you’re still giving them after that? You’re not a parent. You’re a liability.
Also, QR codes? Finally. Took long enough. My kid’s label had a QR code last time. Scanned it. Video showed me how to draw up the dose. No words. Just motion. Perfect. We need more of this. Not more pamphlets. More videos.
Stop trusting ‘common sense.’ It’s the reason 1.3 million people get hurt every year. This isn’t opinion. It’s data. And the data says: use mL. Use the tool. Use the zero. Don’t be the reason your kid ends up in ICU because you thought ‘it’s fine.’
Roisin Kelly
January 22, 2026 AT 11:40This whole thing is a scam. The FDA doesn’t care about your kid. They care about lawsuits. They forced milliliters so pharmacies can blame YOU when something goes wrong. Who’s gonna check if your syringe is calibrated? No one. The system’s rigged.
And ‘leading zero saves lives’? LOL. That’s a myth made up by people who profit off fear. I’ve given my kid .5 mL for years. No issues. You think the drug companies want you to be scared? They do. They make more money when you panic and buy new bottles.
Also-why do I need a QR code to measure 5 mL? Are we turning parents into robots? Next they’ll make us scan a barcode before we breathe.
My kid’s fine. Your fear is not my problem.
And why is everyone acting like this is new? My mom gave me liquid medicine with a spoon in the 80s. I’m alive. So are you. So stop the panic.
They’re just trying to make you feel dumb so you’ll buy their ‘dosing cups’ for $12.99. Real helpful, guys.
Malvina Tomja
January 22, 2026 AT 20:53It is not merely advisable-it is an ethical imperative-to adhere strictly to milliliter-based dosing protocols. The normalization of household utensils as medical instruments constitutes a gross violation of clinical safety standards. The absence of a leading zero is not merely an orthographic oversight; it is a cognitive hazard that directly correlates with iatrogenic harm.
Furthermore, the persistence of ‘tsp’ on labels, even in 2024, reflects a systemic failure of regulatory enforcement. Pharmacies that violate this standard are not merely negligent-they are complicit in medical malpractice.
Concentration misinterpretation remains the most prevalent error among lay caregivers. The conflation of total volume with single-dose volume is not ignorance-it is a failure of education. This is why the teach-back method is not optional. It is mandatory.
And while QR codes are a step forward, they are a Band-Aid on a hemorrhage. The real solution is mandatory pharmacist counseling at point of dispensing. Not a video. Not a pamphlet. A human being. Who looks you in the eye. And asks you to repeat it back.
Until then, we are not saving lives. We are merely delaying tragedy.
Samuel Mendoza
January 24, 2026 AT 18:04Glenda Marínez Granados
January 26, 2026 AT 02:56So let me get this straight. We’ve turned parenting into a compliance exam?
‘Scan the QR code. Check the zero. Don’t breathe wrong.’
Next they’ll make us sign a waiver before we hug our kids.
😂
Meanwhile, I’m over here giving my kid 0.5 mL with a dropper I found in a drawer from 2017. And guess what? He’s still alive. And he’s got better instincts than half the FDA.
Maybe the real problem isn’t the label. Maybe it’s that we’ve forgotten how to trust ourselves.
Also-why does this feel like a cult manual? ‘The Five Sacred Rules of Liquid Medicine.’
Just… chill. Kids have survived worse. Like your ex’s cooking.
Yuri Hyuga
January 27, 2026 AT 16:21Let me tell you something-this is the kind of post that changes lives. 🙌
I used to use spoons. My daughter had a fever last winter. I gave her ‘a teaspoon’ because I thought it was fine. She got worse. We went to the ER. Turns out I gave her 7 mL instead of 0.5 mL. I was terrified.
That day, I learned. I asked the pharmacist for a syringe. They gave me two. Free. They showed me how to draw it up. I practiced. I still use it every time.
Now I tell everyone I know. This isn’t just info-it’s a lifeline. And if you’re reading this and you’re scared? You’re not alone. But you’re also not powerless.
Ask. Learn. Use the tool. You’ve got this. 💪❤️
And if you’re a pharmacist reading this? Thank you. You’re the real heroes.
MARILYN ONEILL
January 28, 2026 AT 01:23Milliliters? Please. I’ve been giving my kid medicine since 2010. I know what a teaspoon is. I’m not an idiot.
And that ‘leading zero’ thing? That’s just a trick to make people feel stupid. I’ve seen labels with 0.5 mL and .5 mL. Same thing. Who cares?
Also-why do I need a QR code? I can’t even scan my own phone without dropping it. My kid’s 2. He’s not gonna help me. This is overkill.
And the 14-day expiry? That’s just a way to sell more medicine. I’ve used liquid Tylenol for months. Still works.
Stop scaring people. We’re not all idiots. Some of us know what we’re doing.
Also-why is everyone acting like this is new? My grandma did it with a spoon and we turned out fine.
Steve Hesketh
January 29, 2026 AT 17:08Brother. Sister. Friend.
I’ve held my daughter while she threw up from a wrong dose. I’ve sat in ER waiting rooms wondering if I killed her. I didn’t. But I came close.
This guide? It’s not perfect. But it’s the truth. And I’m telling you-don’t wait until it’s too late.
I used to think I knew. I thought I was careful. Turns out, I was lucky.
Use the syringe. Even if it’s messy. Even if your hands shake. Even if you’re tired. Even if you’re mad. Even if you’re broke. The pharmacy will give you one for free. Just ask.
And if you’re scared to ask? I get it. I was too.
But you’re not alone. We’re all learning. And we’re all trying. That’s enough.
Love you. Stay safe.
shubham rathee
January 31, 2026 AT 04:08Milliliters only is correct but you missed something
Why are you assuming everyone has access to a syringe or dosing cup
What about people who live in rural areas or can't afford to go to pharmacy
My cousin in Bihar gave medicine with a spoon and her kid is fine
Also concentration is not always printed clearly even in US pharmacies
So your guide is good but it's for privileged people
Real problem is healthcare inequality not spoon usage
Also I use .5 mL and never had issue
So stop being so rigid
Maybe your system is wrong not the people
MAHENDRA MEGHWAL
February 1, 2026 AT 16:52It is imperative to emphasize the necessity of adherence to standardized dosage nomenclature in pediatric pharmacotherapy. The absence of a leading zero constitutes a critical orthographic deviation that has been empirically correlated with increased rates of iatrogenic harm. Furthermore, the use of non-standardized measuring instruments, such as household utensils, introduces unacceptable variability into the administration protocol.
It is further recommended that caregivers engage in the teach-back methodology as a cognitive reinforcement strategy to ensure comprehension. This approach is endorsed by the American Society of Health-System Pharmacists and has demonstrated efficacy in reducing error rates by over 75% in controlled studies.
Pharmaceutical institutions must be held accountable for the dissemination of compliant labeling. Non-compliance should be reported to the appropriate regulatory authority. Vigilance is not optional. It is a moral obligation.
Thank you for this comprehensive and clinically grounded exposition.
Kevin Narvaes
February 1, 2026 AT 19:56ok so i read all this and now i’m scared to even look at medicine
what if the syringe is wrong
what if the pharmacist is lying
what if the zero is there but the ink faded
what if my kid hates syringes and cries
what if i drop it and the whole thing spills
why does everything have to be so hard
can’t we just give them a spoon and pray
i miss the 90s
they didn’t have qr codes back then
and we all lived
…
but also… i’ll use the syringe
just in case
…
thx
Melanie Pearson
February 1, 2026 AT 22:13These guidelines are not suggestions-they are federal mandates. Any pharmacy that fails to comply is violating the Food, Drug, and Cosmetic Act. The FDA does not issue these rules lightly. They are based on peer-reviewed data, not opinion.
Furthermore, the notion that ‘my grandmother did it with a spoon’ is not a defense-it is a relic of pre-regulatory negligence. We have evolved. We have data. We have technology.
Those who resist these standards are not ‘independent thinkers.’ They are endangering children under the guise of tradition.
And for those who claim ‘I’ve never had an issue’-you are statistically lucky, not correct. One mistake is all it takes.
This is not about fear. It is about responsibility. And if you cannot meet that standard, you should not be administering medication.
Period.
Rod Wheatley
February 2, 2026 AT 15:43YES. YES. YES.
Thank you for this. I’ve been screaming this for years.
I work in a pharmacy. I’ve watched parents cry because they think they gave too much. I’ve held their hands while we re-measured. I’ve given out 200 free syringes this month alone.
And you know what? Most of them didn’t even know they were supposed to get one.
So please-don’t just read this. Share it. Send it to your mom. Your sister. Your friend who just had a baby.
And if you’re a pharmacist-don’t wait for them to ask. Hand them the syringe. Say: ‘Here. Let me show you.’
This isn’t just medicine. It’s love.
And love doesn’t guess.
Love measures.
❤️🩺
Uju Megafu
February 4, 2026 AT 12:32Okay but why are we blaming parents?
Why isn’t the pharmacy getting fined for printing ‘tsp’?
Why aren’t they being shut down?
Why do we have to be the ones to fight for basic safety?
Why is it on ME to know the difference between 0.5 and .5?
Why isn’t the system doing its job?
And why are we all just accepting this?
It’s not me being careless.
It’s them being lazy.
And now I have to be a detective just to give my kid Tylenol?
That’s not safe.
That’s broken.
Jarrod Flesch
February 6, 2026 AT 01:53Just wanted to say-this is the kind of post that makes me proud to be a parent.
Not because I’m perfect. I’ve messed up. I’ve used a spoon once. Felt like a monster afterward.
But I learned. I asked. I got the syringe.
And now I carry it in my diaper bag like a superhero tool.
My kid’s 3. He doesn’t like syringes. So I let him ‘help’-he pushes the plunger slowly. Makes it a game.
It’s not about being perfect.
It’s about trying.
And if you’re reading this and you’re scared?
You’re doing better than you think.
❤️
Also-QR codes? Genius. My local pharmacy added them. I scanned one last week. Video showed the syringe angle. Took 12 seconds. I cried.
Thank you for making this so clear.
Stephen Rock
February 7, 2026 AT 12:41Re: Uju’s comment-exactly. The system is broken. But if we wait for it to fix itself, kids die.
I called my pharmacy. Said: ‘Your label says ‘tsp.’ I’m returning this.’ They re-labeled it. No argument.
So don’t wait for a law. Use your voice.
It’s not ‘being difficult.’ It’s being alive.
And if you think ‘my kid’s fine’-that’s not luck. That’s a miracle. And miracles aren’t a strategy.
Do the thing. Even if it’s awkward.
Even if they roll their eyes.
Even if you feel like a nag.
It’s worth it.
Yuri Hyuga
February 8, 2026 AT 17:54To shubham rathee: You’re right. Not everyone has access. That’s why I volunteer with a nonprofit that delivers free dosing tools to rural clinics and low-income families. We’ve sent over 3,000 syringes this year.
If you’re in a place where pharmacies are far or expensive-DM me. I’ll help you get one.
This isn’t about privilege. It’s about justice.
And we can fix this-together.
❤️🩺