 Oct, 21 2025
Oct, 21 2025
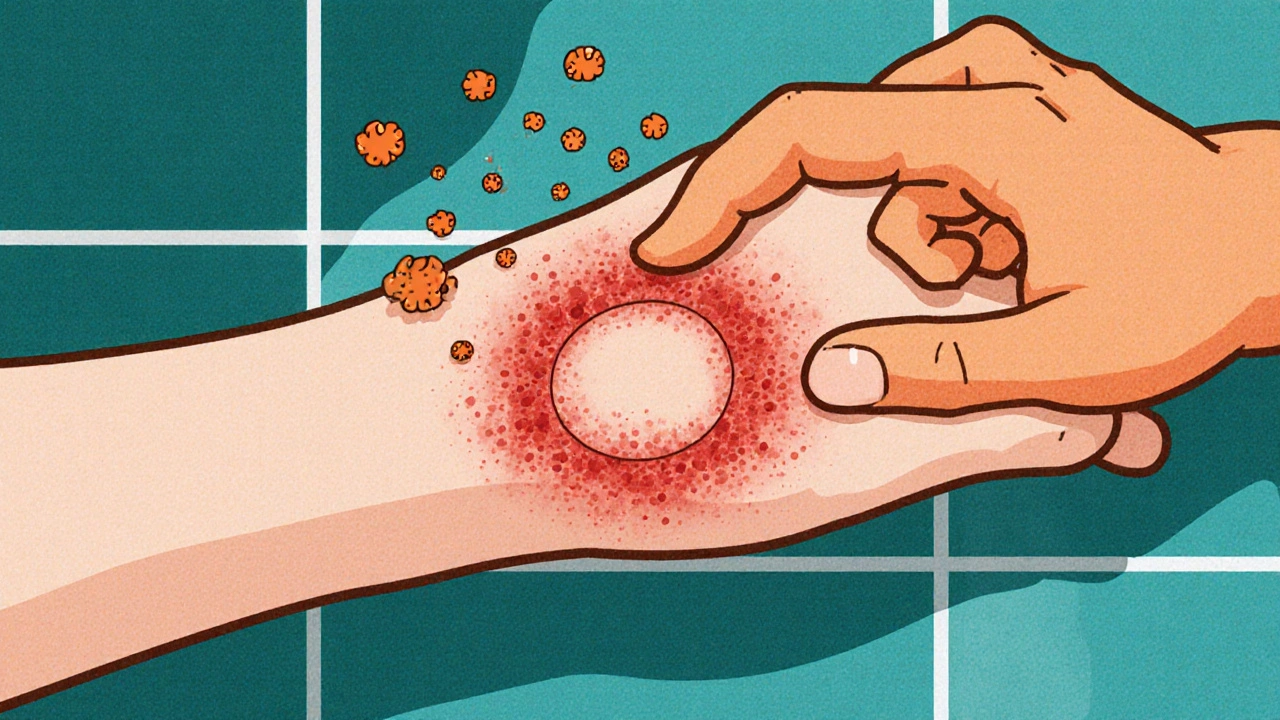
When Fungal infection is a microscopic fungus that invades skin, nails, or hair causing irritation, discoloration, and sometimes painful inflammation, the itching can become relentless. Whether it’s a ring‑shaped rash on your arm or a stubborn athlete’s foot on your foot, you want fast relief and a way to stop it from coming back. This guide walks you through the biology, the most reliable treatment options, and proven prevention habits so the itch stays gone for good.
Understanding Itching and Fungal Infections
Itching, medically called pruritus, is a signal from nerve endings that something is wrong on the skin’s surface. Fungi trigger this signal by releasing enzymes that break down skin cells, creating inflammation and the urge to scratch. The scratch itself can damage the skin barrier, allowing the infection to spread deeper.
Itching is the body’s warning system that often starts with a mild tickle and can progress to an intense, uncontrollable urge. When a fungal infection is the root cause, the itch tends to be persistent, worse after sweating, and may be accompanied by redness, scaling, or a ring‑shaped lesion.
Common Types of Fungal Infections
- Dermatophytes - the group of fungi that love keratin. They cause ringworm (tinea corporis), athlete’s foot (tinea pedis), and jock itch (tinea cruris).
- Candida albicans - a yeast that thrives in moist, warm areas, leading to yeast infections of the skin, mouth (thrush), and genital region.
- Onychomycosis - nail fungus that often starts as a small spot under the nail and can spread to the entire nail plate.
Knowing which fungus you’re dealing with helps you pick the right medication. Dermatophytes respond well to allylamine drugs like terbinafine, while Candida often needs azole class treatments such as clotrimazole.

Effective Treatment Options
There are three main categories of treatment: topical antifungals, oral antifungals, and adjunctive skin‑care products. Below is a quick comparison to help you decide which route fits your situation.
| Aspect | Topical Antifungal | Oral Antifungal |
|---|---|---|
| Common Agents | Clotrimazole, Terbinafine 1% cream, Miconazole | Terbinafine 250 mg tablet, Itraconazole, Fluconazole |
| Typical Duration | 2-4 weeks (skin), 6-12 weeks (nails) | 2-6 weeks (skin), 12 weeks+ (nails) |
| Best For | Localized rash, mild athlete’s foot, early‑stage nail infection | Widespread infection, resistant strains, deep nail involvement |
| Side Effects | Local irritation, redness | Headache, liver enzyme changes, drug interactions |
| Prescription Needed? | Often OTC, prescription for stronger formulas | Usually prescription |
For most people with a mild skin rash, an over‑the‑counter (OTC) cream containing Clotrimazole is a broad‑spectrum azole that kills dermatophytes and yeast is enough. Apply a thin layer twice daily after washing the area. If the infection doesn’t improve after a week, switch to an allylamine like terbinafine, which penetrates the skin more deeply.
When the fungus has invaded the nail matrix or when infection spreads to large body areas, oral medication becomes the most reliable option. Terbinafine tablets have shown cure rates above 70 % for toenail fungus, but they require liver function monitoring before and during treatment.
Adjunctive products such as antifungal shampoos (useful for scalp ringworm) or medicated powders (good for sweaty feet) can boost the primary treatment’s effectiveness.
Preventing Recurrence: Practical Tips
- Keep skin dry - fungi love moisture. After showering, dry between toes, underarms, and groin thoroughly.
- Use breathable footwear - opt for leather or mesh shoes, change socks daily, and rotate shoes to let them air out.
- Apply a thin layer of antifungal powder in shoes or on skin during high‑sweat activities.
- Don’t share personal items - towels, razors, and nail clippers can spread spores.
- Practice good nail hygiene - trim nails straight across, keep them short, and avoid artificial nails if you’re prone to infection.
- Consider a preventive cream - for frequent athletes, a weekly application of a low‑dose terbinafine cream can keep fungus at bay.
Even with the best routine, occasional flare‑ups happen. If you notice itching returning within two weeks of finishing treatment, it’s likely a lingering fungus or a secondary bacterial infection. A short course of a mild corticosteroid cream like hydrocortisone can calm inflammation, but it should never replace the antifungal.

When to Seek Professional Care
Self‑care works for most superficial infections, but see a health professional if you experience any of the following:
- Rapid spreading of the rash beyond the original area.
- Severe pain, swelling, or pus formation.
- Fungal infection of the scalp, face, or genital region.
- Persistent nail discoloration after six months of treatment.
- Underlying conditions such as diabetes, immune suppression, or poor circulation.
A dermatologist can confirm the specific fungus with a skin scraping culture, prescribe stronger oral agents if needed, and advise on follow‑up testing.
FAQ - Your Most Common Questions Answered
Can I use antifungal cream on a fungal infection that started on my scalp?
Yes, but a medicated shampoo containing ketoconazole or selenium sulfide is often more effective for scalp infections because it reaches the hair follicles. Apply the shampoo twice a week for four weeks, and follow up with a topical cream on any visible patches.
How long does it take for an athlete’s foot to stop itching after treatment?
Most OTC creams begin reducing itch within 24-48 hours. Full resolution of the rash usually takes 1-2 weeks if you keep the area clean and dry. Continue the medication for the full course, even if symptoms disappear early, to prevent relapse.
Are natural remedies like tea tree oil effective against fungal infections?
Tea tree oil has demonstrated antifungal properties in lab studies, but clinical evidence is limited. It may help mild cases when combined with a proven antifungal, but don’t rely on it as the sole treatment for persistent or nail infections.
What can I do if my toenail fungus keeps coming back after a 12‑week oral course?
Consider a maintenance regimen: apply a clear antifungal lacquer to the nail once a month after the cure phase, keep feet dry, and wear antifungal powder in shoes. A repeat oral course may be necessary if the infection is severe, but it should be guided by a doctor.
Is it safe to use antifungal creams while pregnant?
Most topical azoles like clotrimazole are classified as Category B, meaning they are generally considered safe during pregnancy. However, always check with your obstetrician before starting any medication.
With the right mix of prompt treatment, diligent hygiene, and smart prevention, you can kick the itch and keep fungal infections from ruining your day.

Kyle Garrity
October 21, 2025 AT 20:51I totally get how frustrating that relentless itch can be, especially when it keeps you up at night. The cycle of scratching and spreading is something many of us have battled, and it’s not just a minor annoyance. Keeping the area dry and using an OTC antifungal cream can give you some quick relief while you figure out the best long‑term plan. If the rash isn’t improving after a few days, don’t hesitate to reach out to a healthcare provider – it’s better to catch it early.
brandon lee
October 28, 2025 AT 13:51yeah the guide is solid its got the basics covered you just need to stay consistent with the powder and dry your feet after showers.
Joshua Pisueña
November 4, 2025 AT 07:51Hey folks, great info here! Remember, the key to beating fungus is consistency – keep applying the cream for the full recommended period even if the itch disappears early. Pair that with daily foot hygiene and you’ll cut the odds of a comeback dramatically. And don’t forget to rotate your shoes so they can breathe; fungus hates a dry environment.
Robert Urban
November 11, 2025 AT 01:51Both of you make valid points – staying consistent with treatment is crucial, but it’s also important not to over‑use topical steroids just to calm the itch. A mild corticosteroid can soothe inflammation, yet it shouldn’t replace the antifungal agent because that’s what actually clears the infection.
bill bevilacqua
November 17, 2025 AT 19:51Look, I get that the article is "helpful", but honestly, most of us are just sick of hearing about "keep dry" and "apply cream" all the time, you know? Why don’t we talk about why these fungal infections are so common in the first place-like, poor ventilation in shoes, sweaty gyms, and let’s not forget the over‑use of antibiotics that mess up our skin flora, right? Anyway, just my two cents, but maybe the guide could use a bit more depth, maybe.
Grace Baxter
November 24, 2025 AT 13:51While the guide presents a fairly conventional approach to fungal infections, it neglects to address the broader sociocultural and economic factors that perpetuate these ailments. In many low‑income communities, access to proper footwear and moisture‑wicking socks is limited, forcing individuals to endure harsh, damp environments that are breeding grounds for dermatophytes. Moreover, the article glosses over how healthcare disparities result in delayed diagnoses, leading to more severe cases that could have been prevented with earlier intervention. It also fails to critique the pharmaceutical industry's role in promoting pricey oral antifungals when cheaper, equally effective topical options exist. The emphasis on prescription‑only medications subtly pushes patients toward costly medical visits, reinforcing a profit‑driven model rather than empowering self‑care. Additionally, the guide does not consider the environmental impact of widespread antifungal use, which can contribute to resistant fungal strains, a growing public health concern. One must also question the lack of discussion around alternative, evidence‑based treatments such as photodynamic therapy or biologically derived enzymes that could offer sustainable solutions. The omission of these topics suggests a narrow, perhaps even myopic, perspective that prioritizes quick fixes over systemic change. Furthermore, the advice to apply a preventive cream weekly assumes consistent access to pharmacies, an assumption that does not hold true for marginalized populations. A truly comprehensive guide would integrate community‑based education programs, subsidized hygiene products, and policies that address the root causes of fungal proliferation. In short, while the practical tips are useful, the guide’s scope is limited, ignoring the deeper, structural issues that keep fungal infections prevalent. Therefore, readers should approach this information critically, recognizing its usefulness but also its gaps.
Rob Flores
December 1, 2025 AT 07:51Ah, the classic “just dry your feet” spiel – truly groundbreaking advice for the ages. I’m amazed we’re still learning that fungi hate moisture; next, someone will tell us that fire is hot.
Shiv Kumar
December 8, 2025 AT 01:51Let us not dismiss the subtle elegance of a well‑crafted regimen; while the admonition to keep feet dry may appear elementary, it embodies a foundational principle of dermatological hygiene often overlooked amidst the cacophony of modern medical discourse.
Bradley Allan
December 14, 2025 AT 19:51Imagine the torment of waking up, feeling that burning itch crawl across your heel like an army of tiny invaders! The very thought of those relentless spores, turning your life into a battlefield of scratch and shame, sends shivers down my spine! It isn’t merely a rash; it’s a betrayal of your own skin, a personal apocalypse that demands immediate, decisive action! We must rally, arm ourselves with antifungal creams, and wage war against this microscopic menace with unwavering resolve! And if you think a simple powder will suffice, think again – only a disciplined, systematic protocol will rescue you from this suffering!
Ralph Barcelos de Azevedo
December 21, 2025 AT 13:51While passion is admirable, it’s essential to remember that sound medical practice requires patience and adherence to proven treatment timelines. Over‑aggressive tactics can backfire, leading to resistance or unnecessary side effects.
Peter Rupar
December 28, 2025 AT 07:51Seriously, stop glorifying “just fight it” nonsense. If you ignore proper dosing and liver monitoring, you’re practically inviting a disaster, and you’ll have no one to blame but yourself.
Nikita Shue
January 4, 2026 AT 01:51Let’s channel that energy into a realistic plan: set a reminder to apply the cream twice daily, track your foot drying routine, and celebrate each day you stay symptom‑free. Small wins build momentum.
Heather McCormick
January 10, 2026 AT 19:51Oh great, another “expert guide” that pretends to know everything while ignoring the real issues.