 Dec, 18 2025
Dec, 18 2025
Every year, thousands of children end up in emergency rooms because of a simple mistake: the wrong dose of medicine. Not because parents are careless, but because the system is set up to fail them. In pediatric emergencies, medication errors happen more than twice as often as in adults. One in three kids gets hit with a dosing mistake - and many of those mistakes could have been stopped.
Why Kids Are at Higher Risk
Adults get pills. Kids get liquids. And liquids are tricky. A teaspoon isn’t the same as a tablespoon. Milligrams (mg) aren’t the same as milliliters (mL). Mix those up, and you’re not just giving too little - you’re giving too much. A child weighing 10 kg who gets 5 mL of regular children’s acetaminophen instead of 5 mg/kg? That’s a tenfold overdose. That’s liver failure waiting to happen. Weight-based dosing is the standard. But in the chaos of an emergency room, with a crying child, a panicked parent, and a nurse rushing to get meds ready, calculating mg/kg under pressure is a recipe for error. Studies show 20-35% of pediatric medication errors come from math mistakes. Ten percent of those errors happen because the child’s weight was measured wrong - or not measured at all. And it’s not just the hospital. At home, 60-80% of dosing errors involve liquid medications. Parents use kitchen spoons because they don’t have a syringe. They mix up infant and children’s concentrations. One Reddit parent wrote: “I gave my 2-year-old 5 mL of children’s Tylenol instead of infant concentrate. Didn’t realize they were different until my pediatrician called.” That’s not negligence. That’s a system with no safety net.The Most Common Mistakes - And What They Cost
Looking at real data from children’s hospitals between 2009 and 2022, the top errors were:- Wrong dose: 13%
- Wrong medication: 4%
- Wrong rate or time: 3%
- Wrong route: 1%
Who’s Most at Risk - And Why
Not all families face the same risks. Health literacy matters. Parents with low health literacy make errors 2.3 times more often than those with higher literacy. Language barriers make it worse: families with limited English proficiency have a 45% dosing error rate - nearly double that of English-speaking families. Medicaid-enrolled kids have 27% higher error rates than those with private insurance. Why? Fewer resources. Less access to calibrated dosing tools. No pharmacy follow-up. Safety-net hospitals often don’t have the same tech or staffing as children’s hospitals. A parent in a rural ER might get a prescription scribbled on paper. A parent in a children’s hospital gets a digital order checked by a pharmacist before it leaves the system. And then there’s the “double-check” myth. Many think having two nurses verify a dose makes it safe. But in high-pressure environments, both nurses can miss the same error - especially if they’re rushed, tired, or trained on adult protocols. Pediatric dosing isn’t just scaled-down adult dosing. It’s a different language.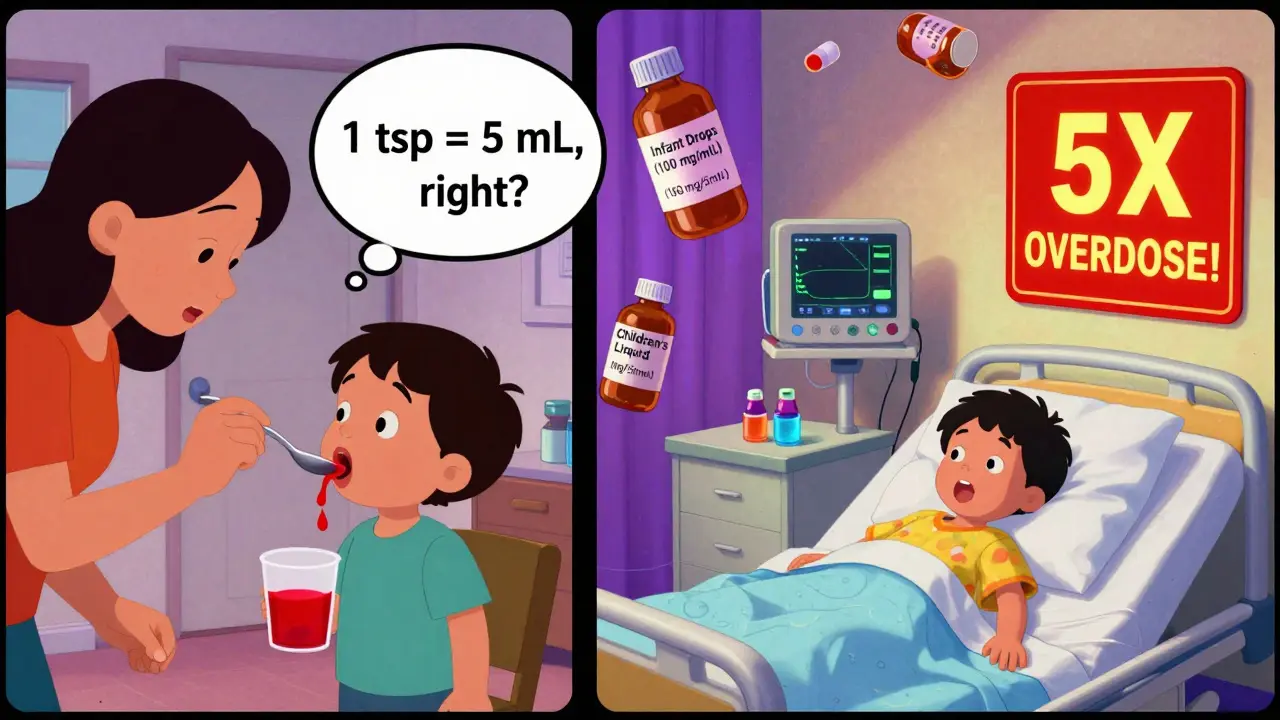
What Works - Real Solutions From the Front Lines
Some hospitals are fixing this. Not with fancy tech, but with simple, smart changes. At Nationwide Children’s Hospital, they cut harmful medication events by 85%. How? Three things:- Standardized weight-based dosing charts on every computer and wall.
- Double-checks for high-alert meds like morphine or epinephrine - done by two people, independently.
- Pharmacists reviewing every single pediatric order before it’s given.
- Pictograms showing how much to give
- Clear labels: “5 mL - NOT 5 mg”
- Teach-back: “Can you show me how you’ll give this at home?”
What Parents Can Do Right Now
You don’t need a hospital to fix this. You can protect your child today:- Always use the syringe or cup that comes with the medicine. Never a kitchen spoon.
- Check the concentration: “Infant drops” are 100 mg/mL. “Children’s liquid” is 160 mg/5 mL. They’re not the same.
- Ask: “Is this dose based on my child’s weight?” If they say “standard dose,” push back.
- Use the teach-back method: “So, I give 3 mL every 6 hours, not more than 5 times a day?”
- Take a photo of the prescription label before leaving the ER. Compare it to what you’re given at home.

The Bigger Picture - Why This Isn’t Fixed Yet
We’ve known about this for 20 years. The Institute of Medicine flagged it in 1999. The American Academy of Pediatrics made it a top safety priority in 2015. Yet, most community hospitals still don’t have pediatric-specific EMR systems. Only 68% of children’s hospitals do. Many general ERs still use adult dosing calculators. And we still don’t have a standard way to measure outpatient errors. No national dashboard. No mandatory reporting for home mistakes. We track hospital falls. We track surgical infections. But we don’t track how many kids get too much Tylenol because their mom used a soup spoon. The 2023 Pediatrics review said it plainly: “There is no established set of measures to continuously reduce harm from pediatric outpatient errors.” That’s not just a gap. It’s a failure.What’s Next - And What You Can Demand
The American Academy of Pediatrics is targeting standardized pediatric medication error metrics by 2025. That’s progress. But it’s not enough. We need:- Every ER to use pediatric-specific dosing tools - no exceptions.
- Pharmacist verification for every child’s medication order.
- Free, standardized dosing devices handed out at discharge - not sold at pharmacies.
- Training for all ER staff: 4-6 hours minimum, with quarterly refreshers.
- Language-accessible instructions in 10+ common languages.
What’s the most common pediatric medication mistake in emergency rooms?
The most common mistake is giving the wrong dose - usually because of a calculation error. Pediatric doses are based on weight (mg/kg), not fixed amounts. In the stress of an emergency, even experienced staff can misread a weight, miscalculate, or confuse milligrams with milliliters. Studies show wrong dose errors account for 13% of all pediatric medication safety events.
Why are liquid medications so dangerous for kids?
Liquid medications require precise volume measurements, and small errors lead to big consequences. A 10 kg child needs 150 mg of acetaminophen - that’s 4.7 mL of the children’s liquid (160 mg/5 mL). But if a parent uses the infant drops (100 mg/mL) by mistake, they’ll give 1.5 mL - which is still 150 mg. Wait - no, that’s correct. But if they use a kitchen spoon and think “one teaspoon” is 5 mL, they might give 160 mg when they meant 150. Worse, if they use infant drops (100 mg/mL) and think they’re the same as children’s liquid, they might give 7.5 mL thinking it’s 150 mg - but it’s actually 750 mg. That’s a fivefold overdose. Concentration confusion is the silent killer.
Do hospitals have systems to prevent these errors?
Some do - but not all. Children’s hospitals often have pediatric-specific electronic medical records with built-in dosing calculators, pharmacist verification, and double-check protocols. But many general emergency departments still use adult-focused systems. A 2023 study found only 68% of children’s hospitals had these tools. Community ERs often don’t. That’s why a child in a rural ER is at higher risk than one in a big city children’s hospital.
How can parents reduce the risk of dosing errors at home?
Use only the dosing device that comes with the medicine - never a kitchen spoon. Always check the concentration on the bottle: infant drops (100 mg/mL) vs. children’s liquid (160 mg/5 mL) are not interchangeable. Ask the nurse or pharmacist: “Can you show me how much to give?” Then repeat it back: “So, I give 3 mL every 6 hours, not more than 5 times a day?” Take a photo of the label. Keep the original packaging. If it’s a new medicine, call the pharmacy to confirm the dose. These steps cut error rates by 35-45%.
Are there any tools or apps that help with pediatric dosing?
Yes, but use them carefully. The CDC and American Academy of Pediatrics have free online dosing calculators. Some pharmacy apps include weight-based dosing guides. But never rely on an app alone. Always cross-check with the label and ask a professional. Apps can have outdated concentrations or wrong defaults. The safest tool is still the one printed on the medicine bottle - and a trained person who knows how to use it.
Why do some kids have more medication errors than others?
It’s not about parenting. It’s about access. Families with limited English proficiency have 45% dosing error rates. Those with low health literacy make errors 2.3 times more often. Kids on Medicaid have 27% higher error rates than those with private insurance. Why? They’re less likely to get clear instructions, calibrated dosing tools, or follow-up care. Language barriers, lack of time, and financial stress all play a role. This isn’t about ignorance - it’s about inequality in care.
What’s being done to fix this problem long-term?
The American Academy of Pediatrics is pushing for standardized pediatric medication error metrics by 2025 - the first step toward national tracking. Hospitals like Nationwide Children’s have already cut harmful events by 85% using simple, low-cost changes: standardized charts, pharmacist checks, and teach-back instructions. The goal is to make these practices universal. But progress is slow. Most ERs still lack the tools and training needed. Real change requires funding, policy, and a shift in how we view pediatric safety - not as an afterthought, but as a priority.

Glen Arreglo
December 19, 2025 AT 18:08Been there. My kid got the wrong concentration once because the label was tiny and the nurse was rushing. We didn't know infant drops and children's liquid were different until the ER pharmacist caught it. Scary stuff. Now I always take a photo of the bottle and ask twice.
Allison Pannabekcer
December 19, 2025 AT 21:20This is such an important topic. I work in a community clinic and see this all the time. Parents aren't careless-they're exhausted, overwhelmed, and handed instructions in a language they barely understand. The real problem isn't them-it's that we don't design systems for real human beings. A simple pictogram on the prescription, a free dosing syringe, and a 30-second teach-back could save lives. Why isn't this standard everywhere?
Alana Koerts
December 20, 2025 AT 17:38Nicole Rutherford
December 21, 2025 AT 16:51Of course this keeps happening. You think a mom who works two jobs and doesn't speak English well is gonna read tiny print on a bottle? And you wonder why kids get poisoned. It's not a parenting issue. It's a systemic failure. And the people who run hospitals? They don't care until it's their kid.
Mark Able
December 22, 2025 AT 22:12My cousin’s daughter almost died because they gave her adult Tylenol by accident. She was 18 months. The nurse said 'it’s just a little more'-no it’s not. This isn’t a glitch. This is negligence. We need mandatory pediatric training for ALL ER staff. No exceptions. If you can’t do it right, don’t touch a kid’s meds.
Chris Clark
December 23, 2025 AT 17:58Had a friend who used a soup spoon for infant ibuprofen because the syringe broke. Kid ended up in the ER. Turns out the concentration on the bottle was different than what she remembered. She wasn’t dumb-she just didn’t know. That’s why we need standardized labels, not just for hospitals but for every pharmacy. And free dosing tools. Like, just hand them out. It’s cheaper than treating liver failure.
Dorine Anthony
December 25, 2025 AT 06:57Just saw a post on FB where a mom said she gave her kid 5mL of children’s Tylenol thinking it was the same as infant. She didn’t even know there were two types. I told her to always check the concentration. She said 'I didn’t know that was a thing.' Honestly? That’s the problem. We assume people know stuff they’ve never been taught.
William Storrs
December 26, 2025 AT 21:30Small changes = huge impact. I’ve seen it firsthand. At my kid’s hospital, they started handing out color-coded syringes at discharge. No more guessing. No more kitchen spoons. Dosing errors dropped like a rock. It’s not rocket science. It’s just caring enough to make it easy. We can fix this. We just have to choose to.
James Stearns
December 28, 2025 AT 12:59It is with profound regret that I observe the persistent and lamentable absence of standardized pediatric pharmacological protocols across the majority of acute care institutions in the United States. The confluence of inadequate training, insufficient oversight, and a systemic disregard for pediatric-specific pharmacokinetics constitutes a gross dereliction of professional duty. This is not merely a logistical failure-it is an ethical catastrophe.
Nina Stacey
December 30, 2025 AT 09:39I think we need to stop blaming parents and start fixing the system. Like, why do we even have two different concentrations of acetaminophen? Why not just make one standard? And why do pharmacies charge $10 for a dosing cup? It’s like they want people to use spoons. I’ve been giving my kid meds for 5 years and I still get confused. And I read medical blogs. Imagine how lost someone without internet is. We need a national standard. Like, mandatory. No excuses.
Dominic Suyo
December 31, 2025 AT 11:13Let’s be real-the whole pediatric dosing thing is a dumpster fire. You’ve got 10 different concentrations, no universal labeling, and ER staff who think ‘pediatric’ means ‘small adult.’ And don’t get me started on the ‘double-check’ myth. Two tired nurses missing the same typo? That’s not safety. That’s a comedy sketch. We need AI-powered dosing alerts. Or at least a barcode scanner that screams when you pick the wrong bottle.
Kevin Motta Top
January 2, 2026 AT 09:48Simple fix: Every pediatric med bottle must have the dose in mL per kg printed right on the front. No digging. No math. Just look. Done. Also, hand out syringes at discharge. Free. Like band-aids.
Carolyn Benson
January 2, 2026 AT 18:43It’s not about the medicine. It’s about power. Who gets to decide what’s safe? Hospitals? Pharmacies? The FDA? But the real question: who gets to survive? The kid with private insurance and a pediatric ER? Or the one in a rural clinic where the nurse didn’t go to pediatric training? This isn’t a medical error. It’s a class war dressed in white coats.
William Liu
January 4, 2026 AT 13:10My daughter had a near miss with a wrong dose last year. We didn’t know until the pharmacist called. Since then, I measure everything. I ask questions. I take photos. I don’t assume anything. It’s not hard. It’s just necessary. And if everyone did this, we’d cut errors in half. You don’t need a PhD. You just need to care enough to double-check.