 Jan, 14 2026
Jan, 14 2026
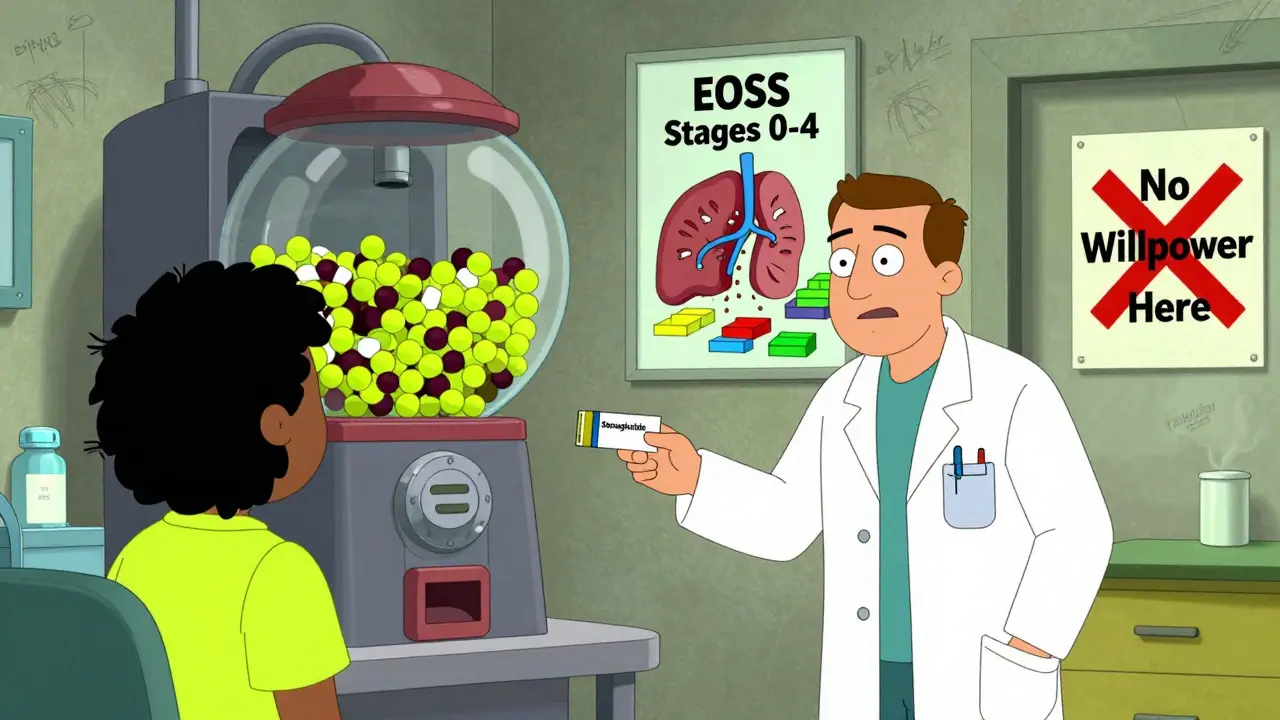
For decades, obesity was seen as a simple matter of eating too much and moving too little. If you just had more willpower, the thinking went, you could lose the weight. But that’s not how the body works-and it’s not how medicine sees it anymore. In 2013, the American Medical Association officially recognized obesity as a chronic disease. Not a lifestyle choice. Not a personal failure. A medical condition with deep biological roots, just like diabetes or high blood pressure.
Why Obesity Is More Than Just Extra Weight
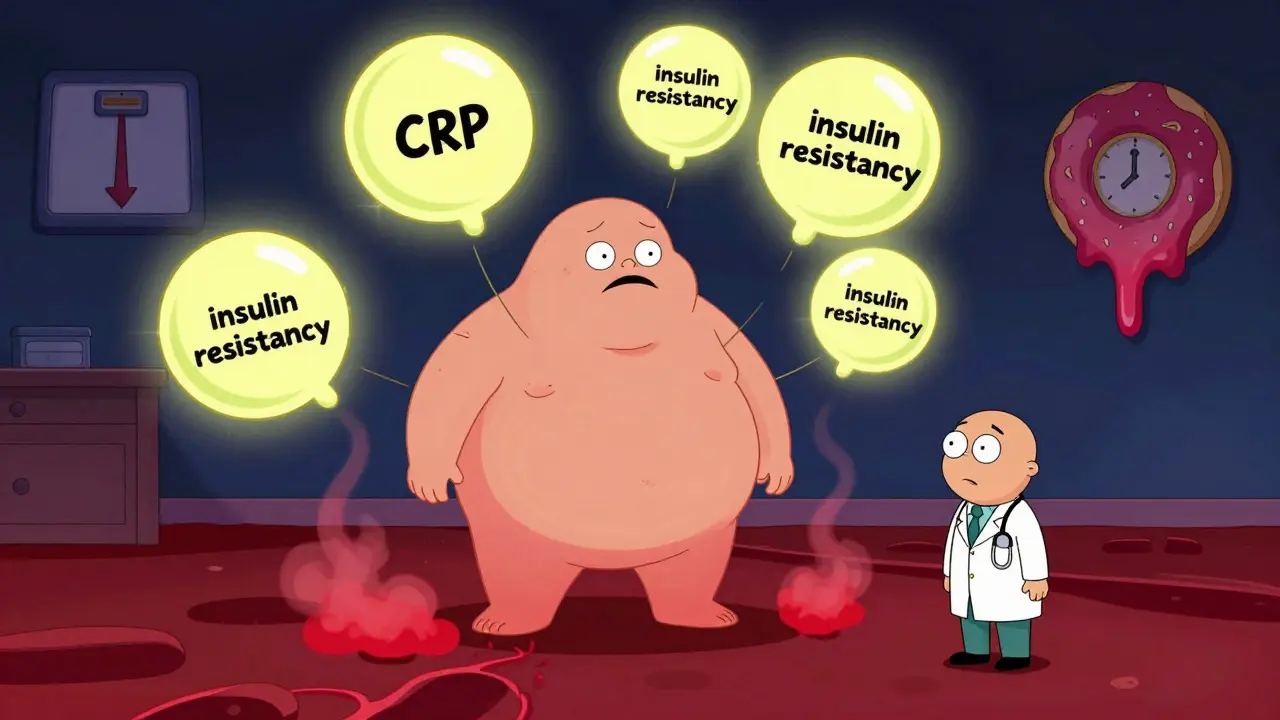
Obesity isn’t just about a number on the scale. It’s about fat tissue that stops functioning properly. When fat cells grow too large and too numerous, they start releasing inflammatory chemicals, disrupting hormones, and interfering with how your body uses insulin. This is called adiposopathy-fat disease. And it’s what turns excess weight into a serious health threat.
People with obesity have, on average, 2 to 3 times higher levels of C-reactive protein, a marker of systemic inflammation. That constant low-grade inflammation damages blood vessels, strains the liver, and increases the risk of type 2 diabetes, heart disease, and at least 13 types of cancer. Visceral fat-the kind that wraps around your organs-is especially dangerous. Studies show it has a strong correlation (r=0.78) with metabolic syndrome, the cluster of conditions that raise your risk of stroke and heart attack.
Genetics play a huge role too. Twin studies suggest 40% to 70% of obesity risk comes from genes. Over 250 genetic variants have been linked to body weight. Some people are born with mutations in the MC4R gene, which controls hunger signals. That’s why two people eating the same diet can have completely different outcomes. It’s not about discipline-it’s about biology.
The Body Fights Back Against Weight Loss
Most people who lose weight eventually gain it back. In fact, research from the University of Michigan shows 90% of people who lose weight through dieting alone regain most of it within five years. Why? Because your body treats weight loss like starvation.
When you lose fat, your body responds by lowering your metabolism and increasing hunger hormones. Ghrelin, the hunger signal, goes up by 15%. Leptin, the hormone that tells you you’re full, drops by 18%. At the same time, your brain becomes more sensitive to food cues-especially high-calorie, high-sugar foods. This isn’t weakness. It’s evolution. Your body is trying to survive.
Obesity also creates its own feedback loop. Extra weight makes movement harder, cutting daily energy expenditure by 15% to 20%. Poor sleep-common in people with obesity-shortens rest by 30 to 45 minutes on average, which further disrupts hunger hormones. Stress raises cortisol, which increases cravings. It’s a cycle that keeps feeding itself.
Metabolic Health Is the Real Goal
Many people focus on weight loss as the only measure of success. But metabolic health is what matters most. You can be overweight and metabolically healthy. And you can be thin and still have insulin resistance, fatty liver, or high blood pressure.
The Edmonton Obesity Staging System (EOSS) helps doctors look beyond BMI. Stage 0 means no health problems, even with a high BMI. Stage 4 means severe organ damage-like heart failure or advanced diabetes. A 2019 Canadian study found that 28.6% of people with obesity were already at Stage 4 when diagnosed. That’s why screening for complications is critical: sleep apnea affects 70% of people with obesity, non-alcoholic fatty liver disease hits 75% of those with BMI over 35, and osteoarthritis risk rises 2 to 3 times for every 5-point increase in BMI.
Improving metabolic health doesn’t always require dramatic weight loss. Losing just 5% to 10% of body weight can significantly lower blood pressure, improve insulin sensitivity, and reduce liver fat. That’s a realistic, life-changing goal-not a number on a magazine cover.

What Actually Works: Evidence-Based Strategies
There’s no magic pill. But there are proven strategies that work when used together.
- Medical nutrition therapy: Working with a registered dietitian trained in obesity care is key. Only about 1,200 such specialists exist in the U.S.-a major access problem. But studies show that structured eating plans, not fad diets, lead to lasting change.
- Physical activity: You don’t need to run marathons. 150 minutes a week of moderate exercise-like brisk walking-improves insulin sensitivity and reduces inflammation. Movement also helps protect muscle mass during weight loss.
- Behavioral counseling: The Obesity Medicine Association recommends at least 14 hours of counseling over six months. Each additional hour adds about 0.23% more weight loss. Therapy helps rewire habits, manage stress, and cope with emotional eating.
- Medication: Five FDA-approved drugs are now available for long-term use. GLP-1 receptor agonists like semaglutide (Wegovy) and tirzepatide (Zepbound) are game-changers. Clinical trials show 15% to 20% average weight loss over a year. Retatrutide, a newer triple agonist approved in 2023, showed 24.2% weight loss in early trials. Side effects like nausea are common but often improve over time.
- Bariatric surgery: For people with severe obesity, surgery remains the most effective long-term treatment. Procedures like gastric bypass and sleeve gastrectomy lead to 25% to 35% weight loss and often reverse type 2 diabetes. But they require lifelong vitamin supplementation and support. About 41% of patients report vitamin deficiencies post-surgery, and 37% say they didn’t get enough follow-up care.
A 2021 Mayo Clinic study found that 72% of people who succeeded long-term used a combination of all these approaches. No single tool works alone. It’s like treating high blood pressure-you don’t just take a pill. You change your diet, move more, manage stress, and take medication when needed.
The Hidden Barriers: Bias, Cost, and Access
Even when people know what to do, getting help is hard. A 2022 survey by the Obesity Action Coalition found 67% of respondents experienced weight bias from healthcare providers. Over half said they were denied medical procedures because of their weight. That stigma keeps people from seeking care.
Cost is another huge barrier. GLP-1 medications can cost $1,000 to $1,400 a month without insurance. Only 37 states require insurers to cover obesity medications. Bariatric surgery costs $15,000 to $25,000, though 87% of qualifying patients get coverage under Medicare. But finding a qualified surgeon is tough-MBSAQIP standards require centers to perform at least 125 procedures a year to ensure safety.
And there’s a workforce crisis. Only 10% of U.S. medical schools require obesity training. To meet demand, the country needs 35,000 more obesity medicine specialists. Right now, most doctors aren’t trained to treat obesity as a disease. They’re trained to tell patients to eat less and move more.
The Future Is Here-But It’s Not Equal
The science has moved forward. The ICD-11 now includes detailed obesity staging that goes beyond BMI. The FDA approved retatrutide in 2023. New research links gut bacteria like Faecalibacterium prausnitzii to obesity severity. Digital tools like app-based coaching show 73% adherence rates in real-world use.
But progress isn’t reaching everyone. Non-Hispanic Black adults have the highest obesity rate at 49.6%, followed by Hispanic adults at 44.8%. Yet access to specialists, medications, and surgery is lowest in these communities. The economic cost of obesity is already $1.72 trillion globally-and could hit $4.32 trillion by 2050 if we don’t change course.
Recognizing obesity as a chronic disease isn’t about giving up. It’s about finally treating it like one. We don’t blame people for having hypertension or asthma. We don’t tell them to just breathe better. We give them tools, support, and medicine. It’s time we did the same for obesity.
Is obesity really a disease, or just a result of poor choices?
Yes, obesity is officially recognized as a chronic disease by the American Medical Association, the World Health Organization, and major medical societies worldwide. It’s caused by complex interactions between genes, hormones, brain signaling, and environment-not simply lack of willpower. The body’s biological systems actively resist weight loss, making it as difficult to maintain as managing diabetes or heart disease.
Can you be overweight and still be metabolically healthy?
Yes. Some people with higher body weight have normal blood pressure, cholesterol, and insulin levels. This is called metabolically healthy obesity. But it’s not permanent. Over time, most will develop metabolic problems. The key is to focus on improving metabolic markers-not just weight. Even a 5% to 10% weight loss can significantly reduce inflammation and insulin resistance.
Why do most diets fail in the long term?
Most diets trigger the body’s starvation response. When you cut calories, your metabolism slows down, hunger hormones rise, and your brain becomes more focused on food. This isn’t a failure of discipline-it’s biology. Studies show 90% of people regain lost weight within five years. Sustainable change requires medical support, behavioral strategies, and sometimes medication-not temporary restrictions.
Are weight-loss medications safe and effective?
FDA-approved medications like semaglutide and tirzepatide are proven safe and effective for long-term use. Clinical trials show average weight loss of 15% to 20% over a year. Side effects like nausea are common at first but usually improve. These drugs work by reducing appetite and slowing digestion. They’re not magic-they work best when combined with healthy eating and movement. They’re also not addictive.
What’s the difference between bariatric surgery and weight-loss drugs?
Bariatric surgery physically changes the stomach and gut, leading to major hormonal shifts that reduce hunger and improve metabolism. It typically results in 25% to 35% weight loss and often reverses type 2 diabetes. Medications like GLP-1 agonists work by mimicking natural gut hormones to reduce appetite. They cause 15% to 20% weight loss and require ongoing use. Surgery is more invasive and permanent; medication is reversible but needs long-term adherence.
Why don’t more doctors treat obesity effectively?
Most doctors weren’t trained to treat obesity as a disease. Only 10% of U.S. medical schools require obesity education. Insurance often doesn’t cover counseling or medication. There’s also deep-rooted stigma-many providers still blame patients. This creates a system where people are told to eat less and move more, even when those steps alone aren’t enough to overcome biology.
How can I find a doctor who treats obesity as a disease?
Look for providers certified by the Obesity Medicine Association (OMA) or board-certified in obesity medicine. These doctors use evidence-based protocols, not quick fixes. You can search their directory online. Ask if they use the Edmonton Obesity Staging System, offer behavioral counseling, and prescribe FDA-approved medications. If they only recommend diets or say you just need more willpower, keep looking.
What to Do Next
If you’re struggling with weight and health, start by asking your doctor for a metabolic health check. Get your blood pressure, fasting glucose, liver enzymes, and cholesterol tested. Ask about sleep apnea and fatty liver disease. Don’t accept a one-size-fits-all diet plan. Demand a personalized approach.
If you’re ready to explore treatment options, find an obesity medicine specialist. Look for programs that combine nutrition, movement, behavioral support, and medication when needed. You don’t have to do this alone. The tools exist. The science is clear. The system is broken-but change is possible.

Jason Yan
January 14, 2026 AT 18:35It’s wild how we still treat fat like it’s a moral failing when the science says it’s a complex metabolic disorder. I mean, we don’t yell at someone with diabetes for eating sugar-we give them insulin. Why is obesity the only chronic disease where we blame the patient? Evolution didn’t design us to live in a world of 24/7 food ads and sedentary jobs. Our bodies are stuck in hunter-gatherer mode while our environment screams ‘eat this, sit there, stress out.’ It’s not willpower. It’s biology on loop.
Vicky Zhang
January 16, 2026 AT 14:26I lost 80 pounds after years of failing diets, and let me tell you-it wasn’t until I found a doctor who actually listened that things changed. I was on GLP-1 meds, therapy, and walking 30 minutes a day. Not because I ‘wanted it bad enough,’ but because my body finally had the tools to stop fighting me. The shame? That was the real weight I had to lose. Nobody tells you how lonely it is when your own family says ‘just eat less.’ You’re not lazy. You’re not broken. You’re just trying to survive a system designed to make you fail.
Susie Deer
January 17, 2026 AT 17:07Obesity is a choice. People eat too much. Move too little. End of story. No more excuses.
TooAfraid ToSay
January 18, 2026 AT 06:14Wait so now if I’m fat I’m not responsible for my actions? That’s the dumbest thing I’ve heard all week. If I can choose to eat a burger, I can choose not to. This whole ‘disease’ thing is just a way for Big Pharma to sell more drugs. Wake up people. Your body is not a broken machine. It’s a tool. Use it right.
Dylan Livingston
January 18, 2026 AT 20:09Oh how touching. Another emotional sob story about how ‘the system failed you.’ Let me guess-you’re one of those people who thinks a $1,400 monthly drug is a ‘right’ and not a privilege? And yet you still refuse to get off the couch? The real tragedy here isn’t the lack of access-it’s the refusal to accept personal accountability. We’ve turned obesity into a victim narrative so we don’t have to face the uncomfortable truth: most people who succeed do so by changing their behavior. Not by waiting for a pill.
Andrew Freeman
January 20, 2026 AT 18:09u mean like how diabetics dont get told to just stop being sugar addicted? yeah its the same thing. its a disease. why do people still think its about willpower. its not. its biology. stop blaming people. its cruel and stupid
Sarah -Jane Vincent
January 22, 2026 AT 00:19GLP-1 drugs are a scam. They’re being pushed by the same corporations that profit from processed food. They’re not curing anything-they’re masking the problem while the real issue-corporate food manipulation-is ignored. And don’t get me started on how insurance companies only cover surgery if you’re ‘morbidly obese’ but deny counseling for ‘mild’ cases. This isn’t medicine. It’s profit-driven control disguised as compassion. Wake up. The system is rigged.
Alvin Bregman
January 22, 2026 AT 03:19i get what you're saying about biology but also i think movement matters. not because you have to burn calories but because moving helps your brain. walking helps me think. stretching helps me sleep. i don't do it to lose weight. i do it because it makes me feel human again. maybe the goal shouldn't be a number on a scale but just feeling okay in your own skin
Allison Deming
January 24, 2026 AT 01:17It is deeply concerning that society has allowed itself to be manipulated into viewing obesity as a medical condition rather than a consequence of moral and behavioral decay. The normalization of excess has eroded personal responsibility and replaced discipline with dependency on pharmaceuticals and surgical interventions. We are not curing disease-we are enabling it. If we continue to remove accountability from the equation, we are not helping anyone-we are merely delaying the inevitable collapse of personal agency in the face of corporate and medical overreach.
Anna Hunger
January 24, 2026 AT 02:32Thank you for this comprehensive, evidence-based breakdown. As a registered dietitian specializing in metabolic health, I’ve seen firsthand how stigma prevents people from seeking help. The Edmonton Obesity Staging System is underutilized but vital-it shifts focus from BMI to clinical outcomes. We need more providers trained in obesity medicine, not just ‘weight loss coaches’ selling keto shakes. And yes, medications like semaglutide are game-changers, but only when paired with behavioral support. The future of obesity care isn’t about willpower-it’s about integrated, compassionate, multidisciplinary care. Let’s stop treating patients like failures and start treating them like people.
Sarah Triphahn
January 24, 2026 AT 02:59So let me get this straight. You’re saying people who are fat are just victims of bad genes and big pharma? What about the people who eat kale and run marathons and still gain weight? Or the ones who eat pizza every day and stay thin? Maybe the problem isn’t the body. Maybe it’s the narrative. You’re giving people an excuse to stay complacent. And that’s worse than obesity.
says haze
January 24, 2026 AT 05:46How ironic that the same people who decry ‘capitalist exploitation’ now demand pharmaceutical subsidies for weight loss. The commodification of biology is the real disease here. We’ve turned human bodies into marketable problems to be solved with branded injections. Meanwhile, real health-sleep, community, joy, movement without performance pressure-is ignored. You don’t need a GLP-1 agonist. You need a life worth living. But that’s too hard to measure, so we give you a pill instead.